Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose:
Rheumatoid arthritis (RA) is associated with an increased risk of cancer compared to the general population. Aging is one of the most important risk factors for the development of cancer in the general population. Aging is also associated with the development of frailty in certain individuals; this is seen even in younger cohorts among patients with RA. Whether a patient’s frailty status confers higher risk of incident cancer or cancer-related mortality in RA remains unexplored.
Methods:
We conducted a retrospective cohort study using the Veterans Affairs Rheumatoid Arthritis (VARA) registry, a multicenter prospective cohort of U.S. veterans with RA, from 2003-2022. The patient’s frailty status at enrollment was defined using the Veterans Affairs Frailty Index (VA-FI) and categorized as robust, pre-frail, and frail. Incident cancers were identified using the Oncology Raw Domain. Patients with prevalent cancer at enrollment were excluded. Separate multivariable Cox proportional hazard models were used to evaluate the association between baseline frailty status with incident cancer and cancer-related mortality, adjusting for age, sex, race, body mass index (BMI), seropositivity for anti-CCP, DAS-28, smoking status, use of prednisone, conventional synthetic (cs) or biologic (b) disease modifying anti-rheumatic drugs (DMARDs). Given the overlap between VAFI and comorbidities, we did not do additional adjustment for comorbidities in final models. The association between frailty and site-specific cancers was also assessed.
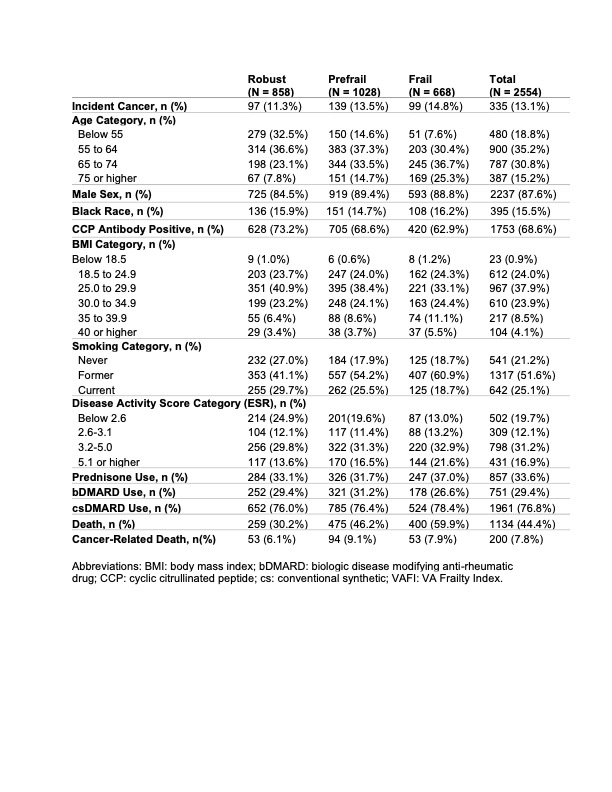
Results: Among eligible patients with RA (n = 2554), 858 were robust (not frail), 1028 were pre-frail, and 668 were frail. A total of 335 (13.1%) incident cancers were identified. Frail individuals were older and had higher rates of death during follow-up compared to robust and pre-frail groups (Table 1).
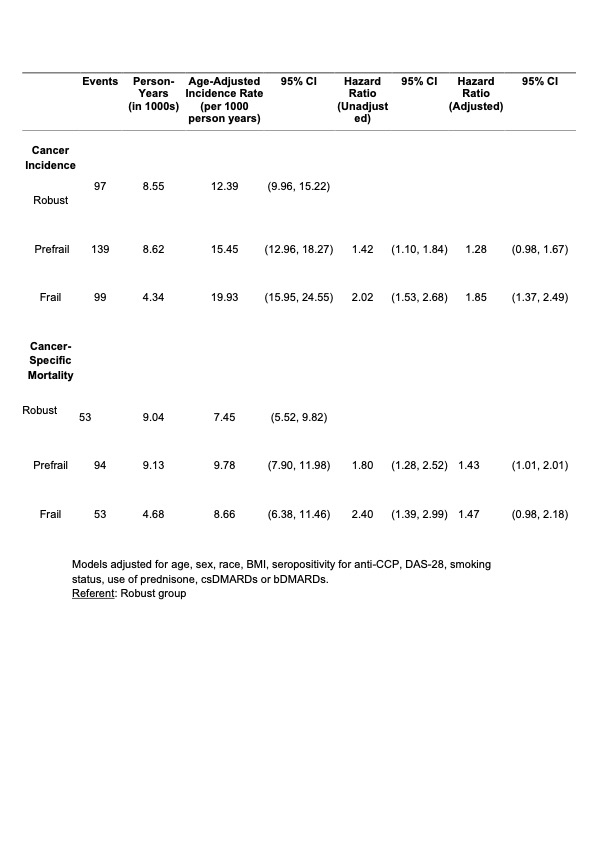
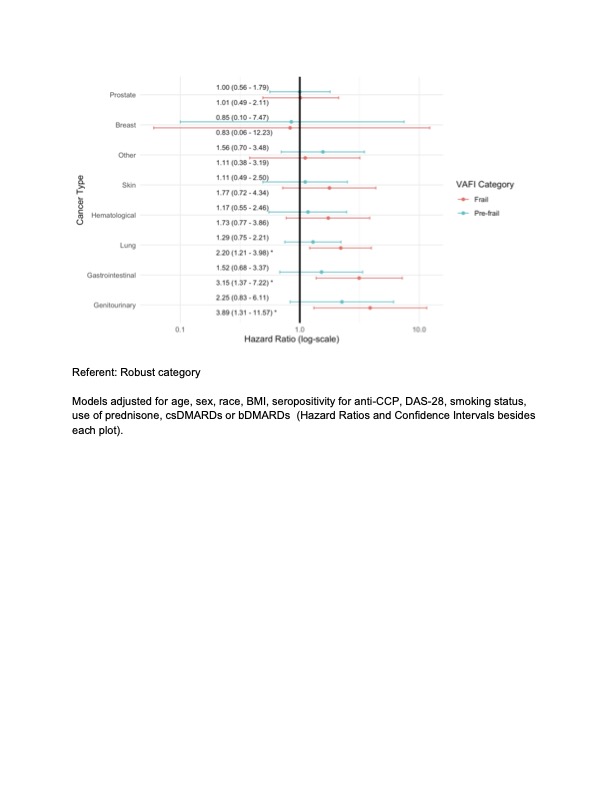
Age-adjusted incidence rates of cancer events were higher among frail individuals, with an age-adjusted incidence rate of 19.93 per 1000 person-years compared to 12.39 and 15.45 per 1000 person-years for robust and pre-frail individuals, respectively. After adjusting for covariates, frailty remained significantly associated with an increased risk of incident cancer (HR 1.85 [95% CI 1.37, 2.49]) compared to the robust group (Table 2). Frailty was also independently associated with an increased risk of certain site-specific cancers, including genitourinary, gastro-intestinal and lung cancers (Figure 1).
In separate multivariable models, pre-frailty was significantly associated with increased cancer-related mortality (HR 1.43, 95% CI: 1.01, 2.01) and frailty showed a trend towards this increased risk (HR 1.47, 95% CI: 0.98, 2.18) (Table 2).
Conclusion: Frailty was an independent risk factor for incident cancer in patients with RA. Pre-frailty and frailty also displayed a trend towards higher cancer-related mortality in these patients. These results underscore the importance of assessing frailty status as a means of risk stratification in RA in addition to suggesting that interventions targeting frailty warrant further investigation as a means of potentially mitigating risk and improving cancer-related outcomes.
To cite this abstract in AMA style:
Bansal B, Baraff A, Wysham K, Andrews J, England B, Mikuls T, Baker J, Michaud K, Meara A, Makris U, Presley C, orkaby a, Singh N. Associations Between Frailty and Incident Cancer and Cancer-related Mortality in Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/associations-between-frailty-and-incident-cancer-and-cancer-related-mortality-in-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-between-frailty-and-incident-cancer-and-cancer-related-mortality-in-veterans-with-rheumatoid-arthritis/