Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: It is not clear whether advances in ANCA-associated vasculitis (AAV) management between 2001-2020 have translated to improvement in population-level outcomes, including among older adults. We hypothesized (1) that more recent calendar time at diagnosis is associated with lower 6-m, 1-y and 5-y mortality and (2) that this improvement is greatest for younger patients, due to higher risk of treatment-associated toxicity in older patients.
Methods: We included Veterans in Veterans Affairs (VA) care between 2001-2020, who met validated International Classification of Diseases (ICD)-9 criteria for microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA), or eosinophilic granulomatosis with polyangiitis (EGPA). We also included Veterans who met ICD-10 based criteria, using corresponding ICD-10 codes. We required ≥ 6 m of VA care and contact ≤ 2 y prior to the index date (date of first ICD code).
The primary endpoint was all-cause 5-y mortality. Patients were censored at last touch date or 9/30/21. Secondary endpoints were 6-m and 1-y mortality. We used multivariable Cox proportional hazards models to test the association between covariates of interest and time to death or censorship.
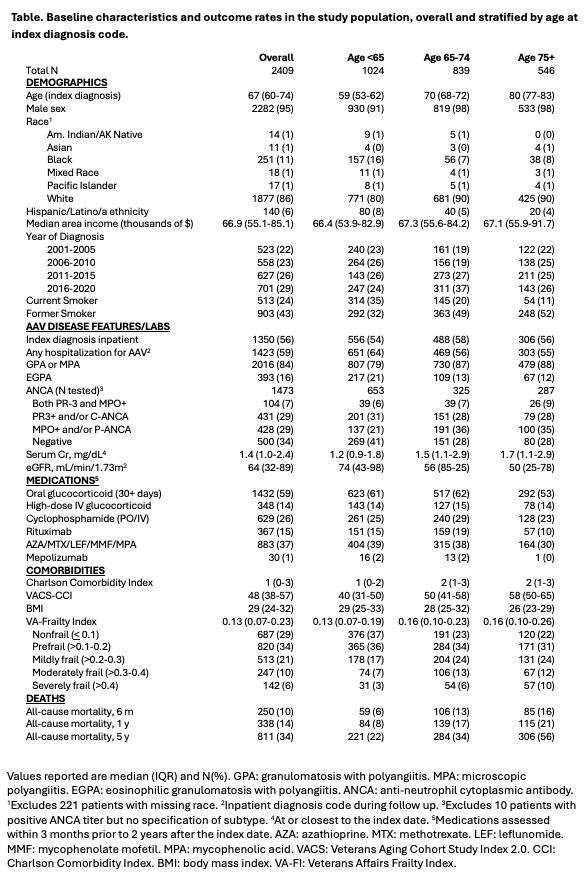
Results: We included 2,409 Veterans, 2,016 of whom had MPA or GPA and 393 of whom had EGPA (Table); most were male (98%) and of White race (86%). Median age at diagnosis was 67 y (IQR, 60-74).
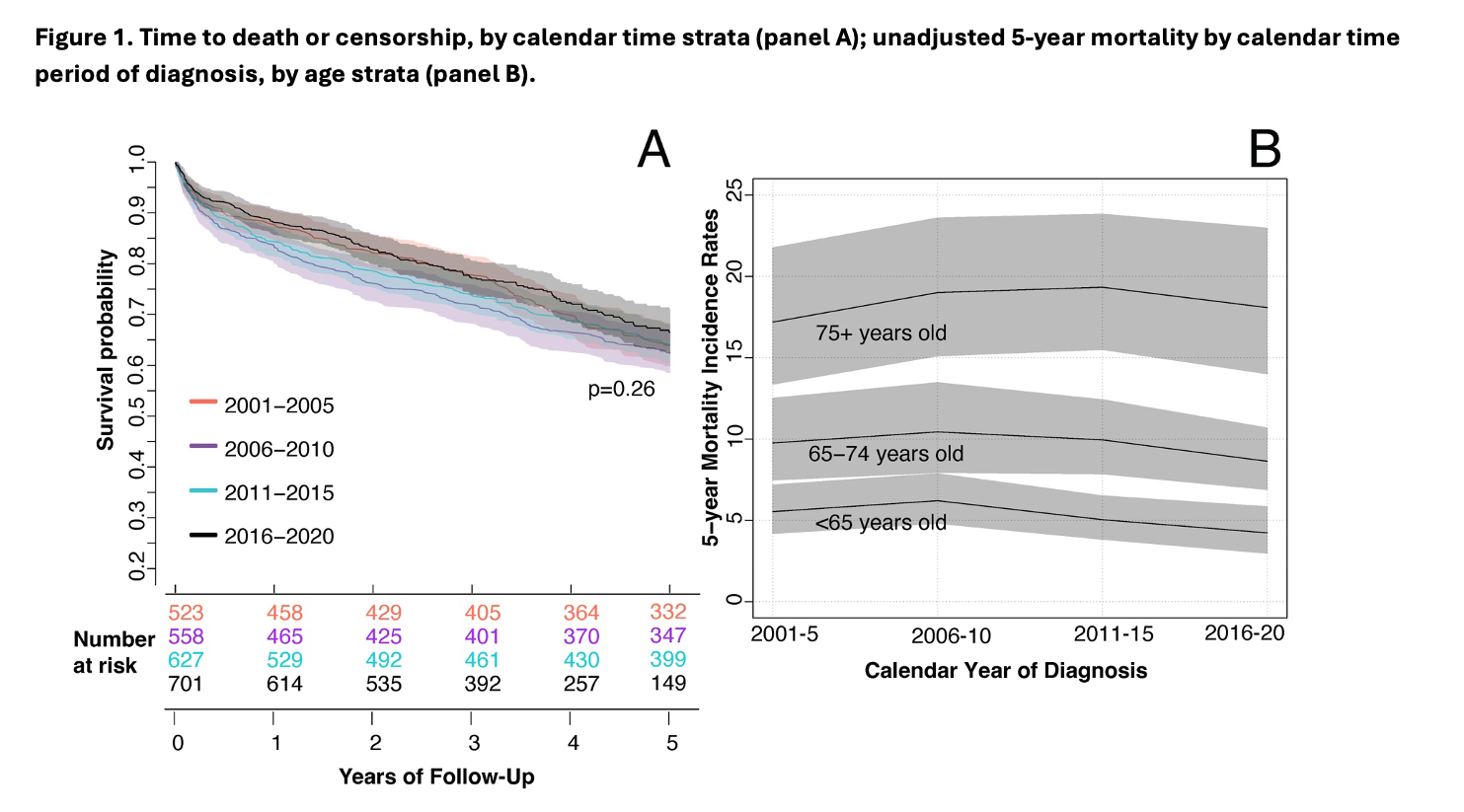
Over a maximum of 5 y, 811 patients died, with 250 deaths at 6 m and 311 at 1 y. The crude 5-y mortality rate did not change significantly over calendar time, including by age at diagnosis subgroups (< 65, 65-74, and 75+ y) (Figure 1A, 1B).
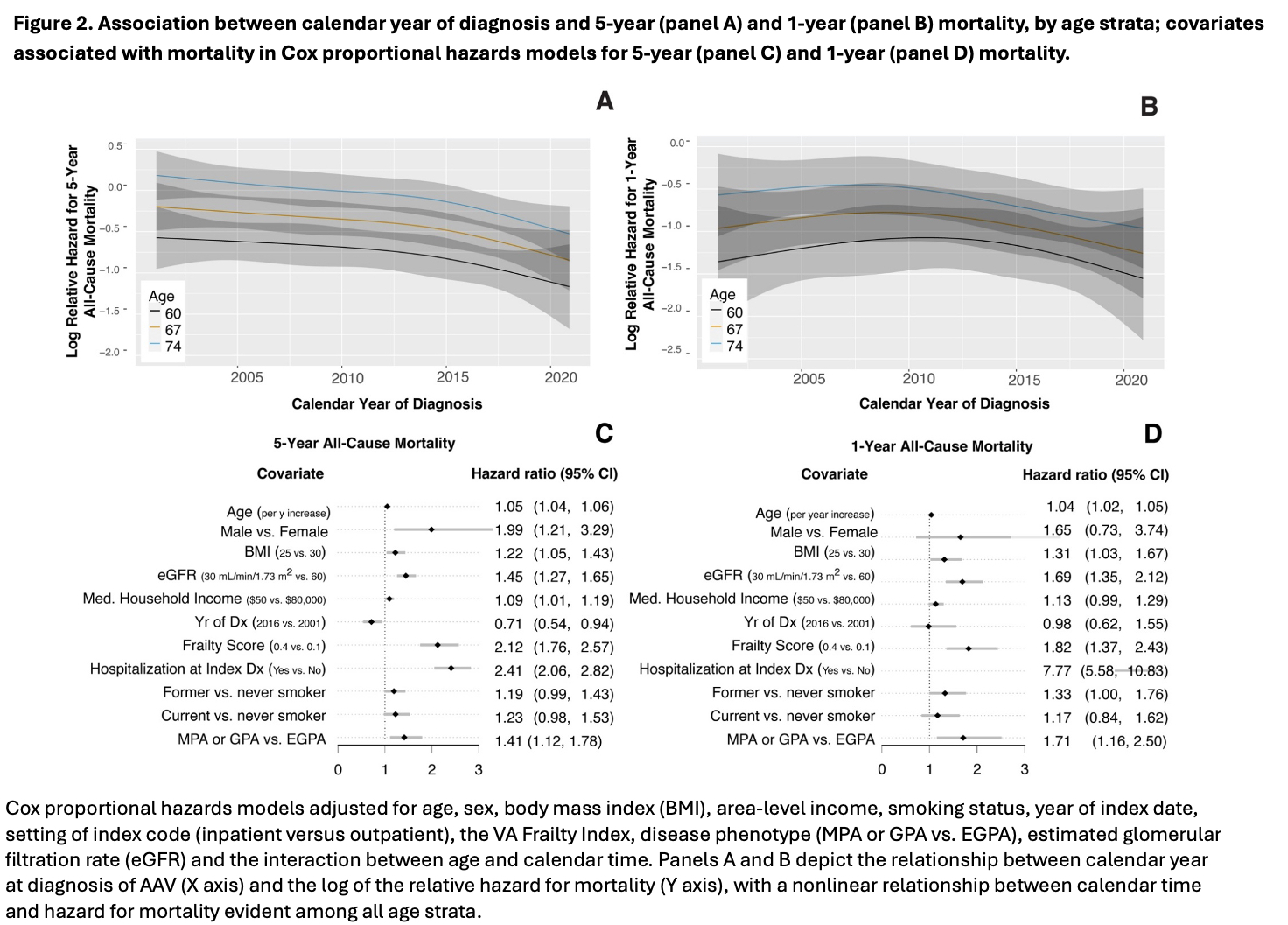
In adjusted models (covariates listed in Fig. 2), calendar year of diagnosis was associated in a nonlinear fashion with 5-y mortality hazard (HR 0.7 for 2016 vs. 2001, 95% CI 0.5-0.9; p=0.005; Fig. 2A) but not with 6-m (HR 0.8, 95% CI 0.5-1.4) or 1-y mortality (HR 1.0, 95% CI 0.6-1.6; Fig. 2B). The association between calendar time and 5-y mortality did not differ by age (p interaction=0.98). Additional baseline factors associated with higher risk of 5- and 1-y mortality included age, sex, inpatient (vs outpatient) index diagnosis, BMI, area-level income, lower estimated glomerular filtration rate (eGFR) at or prior to diagnosis, higher frailty, and MPA or GPA vs EGPA (Fig. 2C, 2D). Results for 6-m mortality were similar except that sex and BMI were not associated with mortality risk.
In analysis stratified by phenotype (MPA or GPA vs. EGPA), risk factors for 5-y mortality in patients with MPA or GPA included age, sex, inpatient index code, year of diagnosis, eGFR, frailty score, and BMI. In contrast, among patients with EGPA, only age, frailty score, and inpatient index code were significantly associated with 5-y mortality.
Conclusion: In this large cohort of mostly male Veterans, diagnosis of AAV during more recent calendar time was associated with lower risk for 5-y mortality. We found no evidence that the association differed by age at diagnosis. Calendar time was not associated with 6-m or 1-y mortality, but lower numbers of events may have limited power for these analyses. Multiple clinical factors including frailty, male sex, kidney function, and lower socioeconomic status were also associated with mortality.
To cite this abstract in AMA style:
Hanberg J, Eden S, Anderson-Mellies A, Kundu S, Freiberg M, Wallace Z, Hsieh E. Associations Between Calendar Time and Age at Diagnosis with Mortality in a National Cohort of Veterans with ANCA-Associated Vasculitis from 2001-2020 [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/associations-between-calendar-time-and-age-at-diagnosis-with-mortality-in-a-national-cohort-of-veterans-with-anca-associated-vasculitis-from-2001-2020/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-between-calendar-time-and-age-at-diagnosis-with-mortality-in-a-national-cohort-of-veterans-with-anca-associated-vasculitis-from-2001-2020/