Session Information
Date: Monday, November 6, 2017
Title: Epidemiology and Public Health Poster II: Rheumatic Diseases Other than Rheumatoid Arthritis
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Ultraviolet-B radiation (UV-B) exposure may lead to worsened photosensitivity, rashes, and systemic flares among SLE patients. Although UV-B radiation damages keratinocytes and may result in production of novel forms of autoantigens, it remains unknown whether UV-B exposure increases the risk of developing SLE. We aimed to examine the association of UV-B exposure with risk of incident SLE in a large prospective cohort of women, examining SLE risk overall and by subtypes defined by presence of anti-Ro/La antibodies (+anti-Ro/La) and/or cutaneous manifestations most associated with UV exposure in SLE patients.
Methods: The Nurses’ Health Study (NHS) enrolled 121,701 U.S. female nurses in 1976; NHSII enrolled 116,430 in 1989. Biennial questionnaires collected lifestyle, environmental, and medical data. Residential addresses were geocoded. Incident SLE was confirmed by medical record review. National Aeronautics and Space Administration Total Ozone Mapping Spectrometer and Ozone Monitoring Instrument gridded remote sensing images scaled to a 1 km spatial resolution predicted average July noon-time erythemal UV-B (mW/m2) annually starting in 1980. Participants without UV-B data at baseline were excluded. Hazard ratios (HR) and 95% confidence intervals (CI) were estimated using Cox regression models across tertiles of cohort-specific, time-varying cumulative average UV-B through one cycle prior to SLE onset. We examined SLE risk overall and stratified by presence of anti-Ro/La or cutaneous manifestations (malar rash and/or photosensitivity) at diagnosis through 2014 (NHS) or 2013 (NHSII), controlling for potential confounders. We also conducted a ‘lagged’ analysis by ending the exposure window two cycles prior to SLE diagnosis, as SLE symptoms may develop insidiously pre-diagnosis.
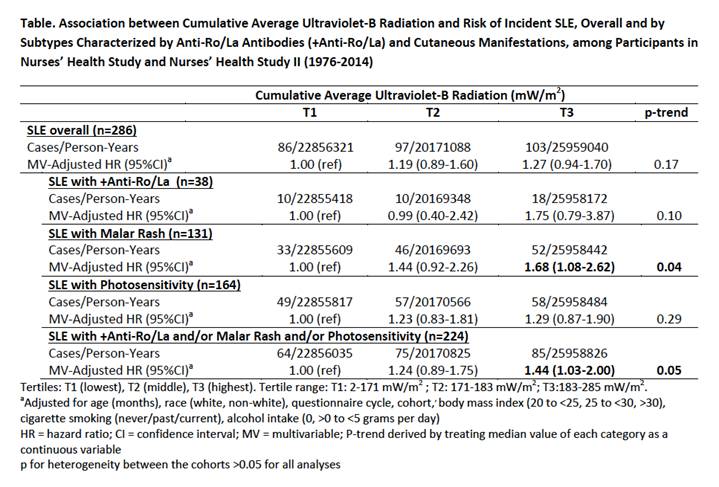
Results: Mean age at SLE diagnosis was 49.3 (10.4) years among 286 SLE cases in NHS/NHSII. At SLE diagnosis, 13% of women had +anti-Ro/La whereas 80% had either +anti-Ro/La or at least one cutaneous manifestation. Compared to the lowest tertile of UV-B exposure, risk of overall SLE, SLE with +anti-Ro/La, or SLE with photosensitivity in the highest UV-B tertile were increased, but not statistically significant in the main analysis (Table) or in lagged analyses. However, women in the highest UV-B tertile had statistically significantly increased risks of SLE with malar rash (HR 1.68 [95% CI 1.08-2.62]) (Table), but this was no longer significant in the lagged analysis (HR 1.41 [95% CI 0.88-2.25]).
Conclusion: Increasing cumulative UV-B exposure was not associated with risk of developing overall SLE. However, among women at risk for SLE, living in areas with higher UV-B exposure was associated with increased risk of developing SLE presenting with malar rash. Further studies are warranted to determine whether high UV-B exposure may play a role in triggering SLE onset with malar rash.
To cite this abstract in AMA style:
Barbhaiya M, Hart J, Malspeis S, Tedeschi SK, Kreps DJ, VoPham T, Sparks JA, Karlson E, Laden F, Costenbader KH. Association of Ultraviolet-B Radiation and Risk of SLE Among Women in the Nurses’ Health Studies [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/association-of-ultraviolet-b-radiation-and-risk-of-sle-among-women-in-the-nurses-health-studies/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-ultraviolet-b-radiation-and-risk-of-sle-among-women-in-the-nurses-health-studies/