Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile dermatomyositis (JDM) is an idiopathic inflammatory myopathy characterized by proximal muscle weakness, a distinct rash, and an increased risk of calcinosis, with long-term negative impact on quality of life. The Bohan and Peter criteria from 1975 require either a muscle biopsy or electromyography, but the 2017 ACR classification criteria do not. There is debate in the field about the utility of the muscle biopsy when weighing the risks of a procedure. In addition to diagnostic value, the muscle biopsy has been shown to be predictive of disease severity, and therefore helpful to inform treatment decisions. The Childhood Myositis Assessment Scale (CMAS) is an internationally validated quantitative assessment tool used to assess muscle function and endurance in patients with JDM. It provides a score from 0-52, with increased numbers indicating greater muscle function. We sought to assess the improvement of muscle performance (i.e., CMAS) in patients who did and did not have muscle biopsies as part of their diagnostic testing.
Methods: This was a single center retrospective cohort study performed at CCHMC. This study was approved by the CCHMC IRB with a waiver of consent for retrospective data collection. Inclusion criteria were: a) definite or probable diagnosis of JDM according to the Bohan and Peter criteria in patients ≤18 years old; b) complete medical records (i.e. medication history, clinical and laboratory history to assess activity and remission) and c) follow-up for JDM of at least 18 months. Patients were excluded if they were diagnosed with other rheumatic diseases associated with myositis.
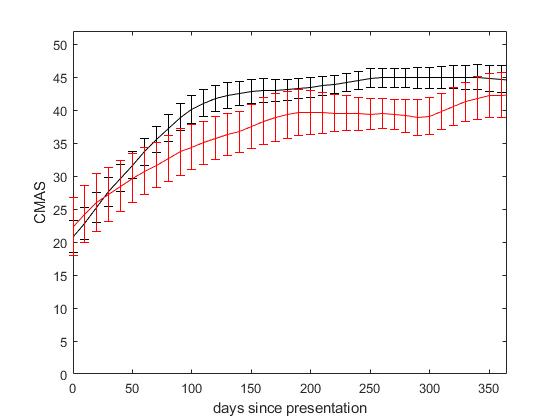
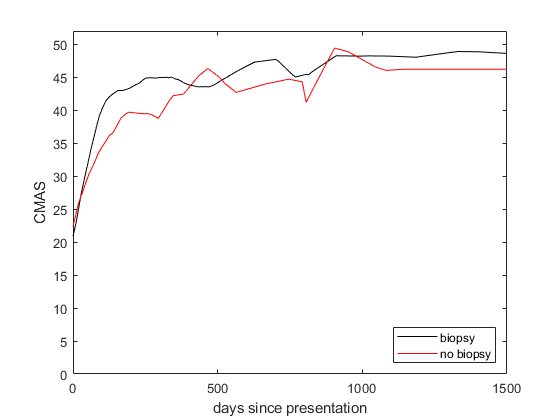
Patients were excluded from analysis if critical information was absent in the database, such as baseline or final visit CMAS values and if information around whether they had a muscle biopsy was missing. Mean CMAS for each group were plotted over time using linear interpolated values, and truncated at 365 or 1500 days, with error bars depicting standard error of the mean.
Results: We identified 49 children with JDM diagnosed between 2006 and 2020, of which 27 had biopsy performed and 22 did not. Patients who presented with lower CMAS were significantly more likely to get muscle biopsy than those with higher CMAS at presentation (average CMAS 30 ± 2.6 vs 40 ± 2.4).
Patients in our cohort who presented with CMAS< 35 and had muscle biopsy (N=15) had a faster functional recovery compared to those who did not have muscle biopsy (N=5), despite a trend toward muscle biopsy at presentation in patients with lower CMAS, and therefore more severe functional disease, with statistically significant clinical improvement at 4 months from diagnosis (Figure 1). On average, this benefit is sustained over time up to 1500 days post-diagnosis (Figure 2).
Conclusion: The functional muscle performance of patients with JDM in our cohort, as measured by the CMAS, recovers more quickly for patients who had muscle biopsy at diagnosis, despite these patients having the same or lower CMAS at presentation. As muscle biopsies provide objective findings predictive of disease severity, this study suggests that treatment decisions may be informed by severity predictors provided through histopathologic analysis.
To cite this abstract in AMA style:
O'Connor S, Maccora I, Quinlan-Waters M, brunner h, Angeles-Han s, schulert g, kottyan l. Association of Muscle Biopsies and Functional Recovery Trajectories in Children with Juvenile Dermatomyositis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-muscle-biopsies-and-functional-recovery-trajectories-in-children-with-juvenile-dermatomyositis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-muscle-biopsies-and-functional-recovery-trajectories-in-children-with-juvenile-dermatomyositis/