Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Characterizing knee symptom (i.e., pain and function) trajectories and understanding differences among symptom trajectories have the potential to promote the development of customized treatment and management plans for patients. We sought to identify diverse knee symptom trajectories in the OAI and to investigate potential associations between baseline MRI structural changes and distinct temporal knee symptom phenotypes.
Methods: We used data from the OAI and employed a two-stage strategy. In Stage 1, we identified knees with at least one of four symptom scores equal to 0 at baseline: WOMAC function score (0-68, none to extreme functional limitation), WOMAC pain score (0-20, none to extreme pain), KOOS knee pain frequency (0-4, none to daily), and the Numerical Rating Scale for knee pain severity (0-10, none to worst pain). We employed group-based multiple-trajectory modeling (GBMTM) to cluster the selected knees into distinct knee pain/function progression trajectories. In Stage 2, we utilized logistic regression models to examine the relationship between the Group 3 knee symptom trajectory identified in Stage 1 vs. Group 1 and Group 2 combined into a reference group, and various MRI-defined features independently, including bone marrow lesions (BMLs), cartilage surface damage, cartilage depth damage, Hoffa-synovitis, and effusion-synovitis (ES), as per the MRI Osteoarthritis Knee Score (MOAKS), in separate models, including age, gender, race, and BMI. The Stage 2 analysis was based on a subsample size of 881 knees for which MOAKS readings were available.
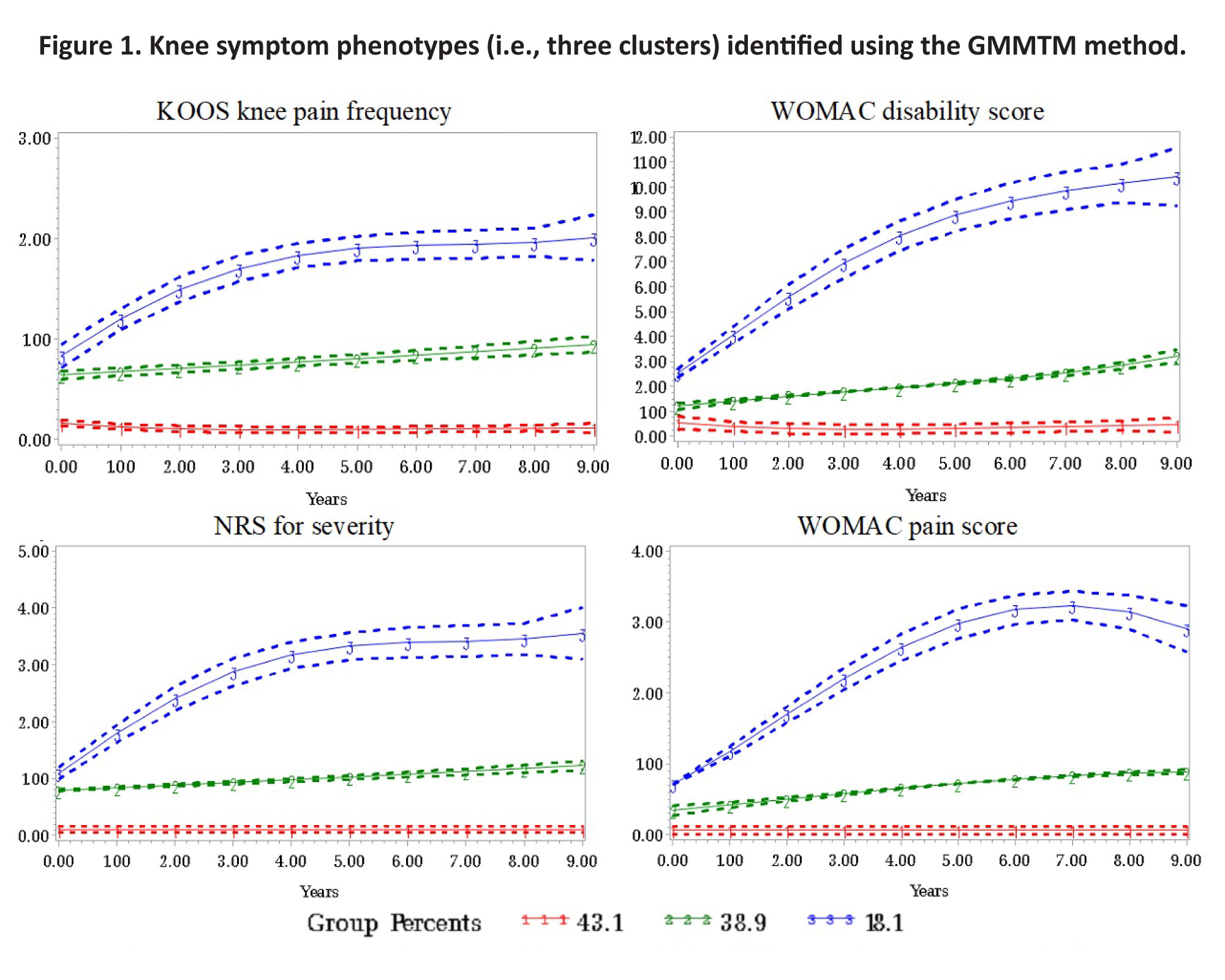
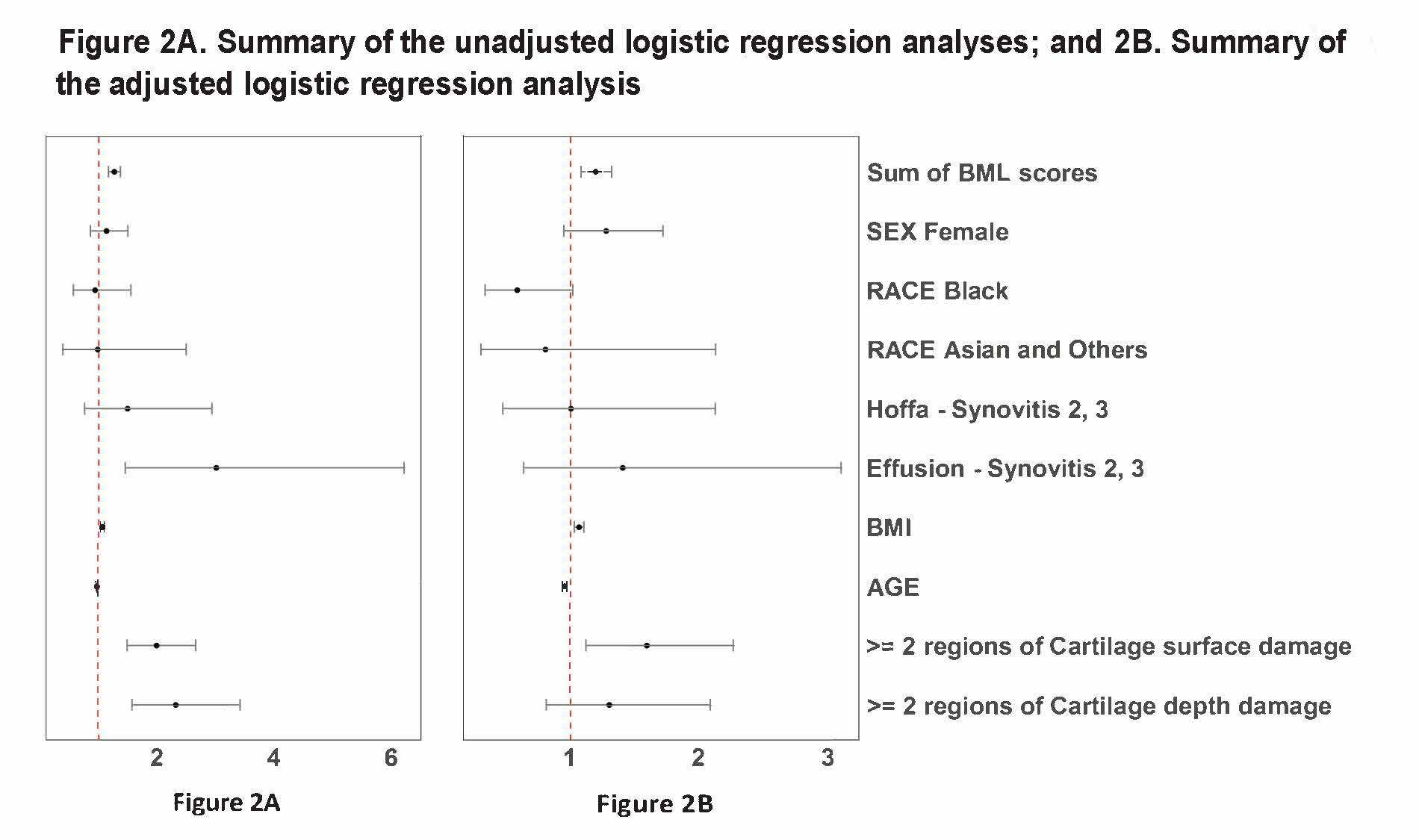
Results: Overall, 3066 knees met our Stage 1 inclusion criteria. Three distinct knee symptom phenotypes were generated by GBMTM (Figure 1): Group 1 (1321 knees) was a non-progressive trajectory; Group 2 (1192 knees) was a slowly progressive trajectory; and Group 3 (553 knees) was a rapid progression trajectory. The forest plot of odds ratios (ORs) for the unadjusted results showed that higher scores for BMLs, effusion-synovitis, cartilage surface damage, cartilage depth damage and higher BMI were associated with the rapid symptom progression phenotype (Figure 2). The forest plot of ORs for the adjusted logistic regression showed that each unit increase in total BML size score corresponded to an OR of 1.20 (95% CI: 1.09, 1.33) for Group 3 vs. Groups 1 and 2; ≥ 2 regions with cartilage surface damage corresponded to an OR of 1.59 (95% CI; 1.12, 2.26). There was a suggestion that advancing age was associated with a lower likelihood of being classified in the fast progression phenotype.
Conclusion: We delineated three distinct knee symptom phenotypes using longitudinal OAI data extending over ten years. Our findings revealed consistent knee symptom trajectories across all four distinct knee symptom measurements. The presence of MRI structural abnormalities (i.e., BMLs and cartilage damage) in the absence of pain or functional limitations may serve as indicators of rapid knee symptom development. Subgroups of patients who have worse knee symptom trajectories may be in greatest need for treatment, while those with minimal or mild symptom trajectories may not need treatment.
Hoffa-synovitis (0, 1 as the referent group), and effusion-synovitis (ES, (0, 1 as the referent group); bone marrow lesions (BMLs, sum of size scores in 15 sub-regions); cartilage surface damage (>= 2 of 14 sub-regions with more than 10% of surface area of the sub-region with cartilage loss), cartilage depth damage (>= 2 of 14 sub-regions with more than 10% of surface area of the sub-region with full-thickness cartilage loss), as graded by the MRI Osteoarthritis Knee Score (MOAKS)
To cite this abstract in AMA style:
Liu S, Doung T, Ge Y, Sun X, Golightly Y, Nelson A, Neogi T, Duryea J, Kwoh K. Association of MRI-Defined Structure Features at Baseline with Knee Pain and Function Trajectories: Data from the Osteoarthritis Initiative (OAI) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-mri-defined-structure-features-at-baseline-with-knee-pain-and-function-trajectories-data-from-the-osteoarthritis-initiative-oai/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-mri-defined-structure-features-at-baseline-with-knee-pain-and-function-trajectories-data-from-the-osteoarthritis-initiative-oai/