Session Information
Date: Sunday, November 12, 2023
Title: (0691–0721) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The association of large vessel vasculitis (LVV), whether Takayasu arteritis (TA) or giant cell arteritis (GCA), with inflammatory bowel disease (IBD) is a rare and challenging condition. The prevalence of LVV in IBD cohorts is less than 1%, but the prevalence of IBD can be as high as 15.4% in TA cohorts, and population-based studies confirmed this association. We aimed to describe the characteristics and outcome of LVV-IBD patients, with a focus on the therapeutic management.
Methods: We performed an observational, multicenter, retrospective case-control study in Western Europe countries (France, Italy, Spain, Germany, Belgium). Cases were adults or children with both LVV and IBD (LVV-IBD), whereas controls had isolated TA (iTA) or GCA (iGCA).
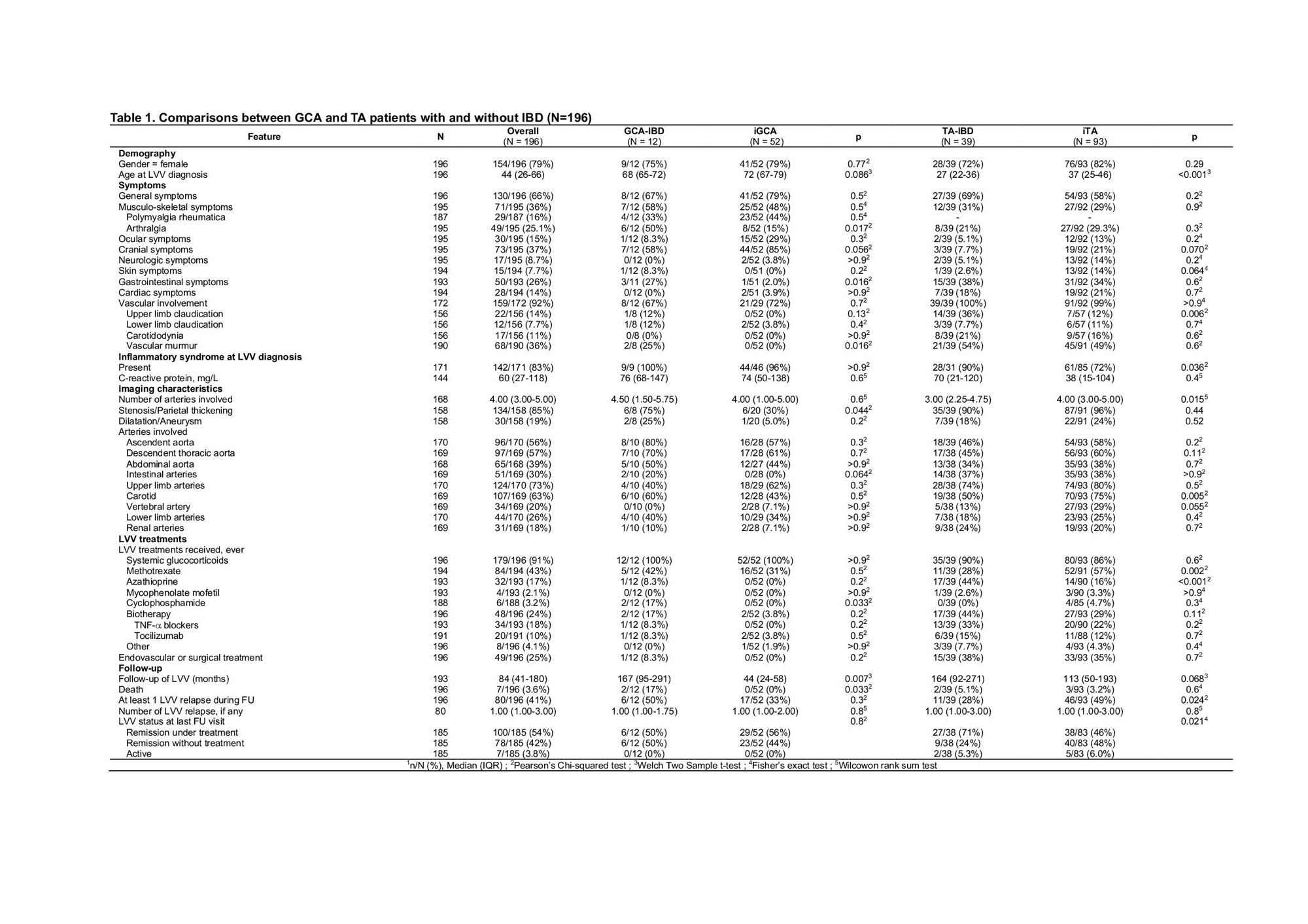
Results: Fifty-one LVV-IBD patients were included, including 39 TA-IBD and 12 GCA-IBD patients, and compared with 93 iTA and 52 iGCA. LVV-IBD patients were mostly females (75% in TA-IBD and 72% in GCA-IBD). Crohn’s disease was more common in TA-IBD (67%), while ulcerative colitis was more common in GCA-IBD (58%). LVV occurred after IBD in most cases (56% in TA-IBD and 75% in GCA-IBD), with a median interval of 1 year in TA-IBD and 8.6 years in GCA-IBD, and were diagnosed concomitantly in 16%. Location, behaviour and complications of IBD were similar to previously reported IBD cohorts.
Compared to iTA patients, TA-IBD patients were significantly younger at TA diagnosis (27 vs. 37 years, p < 0.001) and had more upper limb claudication (36 vs 12%, p=0.006). The number of affected arterial segments was lower in TA-IBD (3 vs. 4 segments, p=0.015) and carotid artery involvement was less common in TA-IBD patients than in iTA patients (50 vs. 75% respectively, p=0.005).
Compared to iGCA patients, GCA-IBD patients had more arthralgia (50 vs 15%, p=0.017) and vascular murmur (25 vs 0%, p=0.016). GCA-IBD patients had more arterial thickening or stenosis than controls (75 vs. 30% respectively, p=0.044).
LVV occurred in IBD patients while on therapy in 77% (86% for TA-IBD and 56% for GCA-IBD), including oral glucocorticoids (GCs) in 36%, azathioprine (AZA) in 25%, or TNF-a blockers in 33% of TA-IBD.
LVV-IBD were treated with GCs in 91%, methotrexate in 43%, AZA in 17% or cyclophosphamide in 3.2%. Biologics were used in 24%, including mainly TNF-a blockers in TA-IBD patients (33%). AZA was used more frequently in TA-IBD patients than in iTA, with the latter mainly receiving methotrexate.
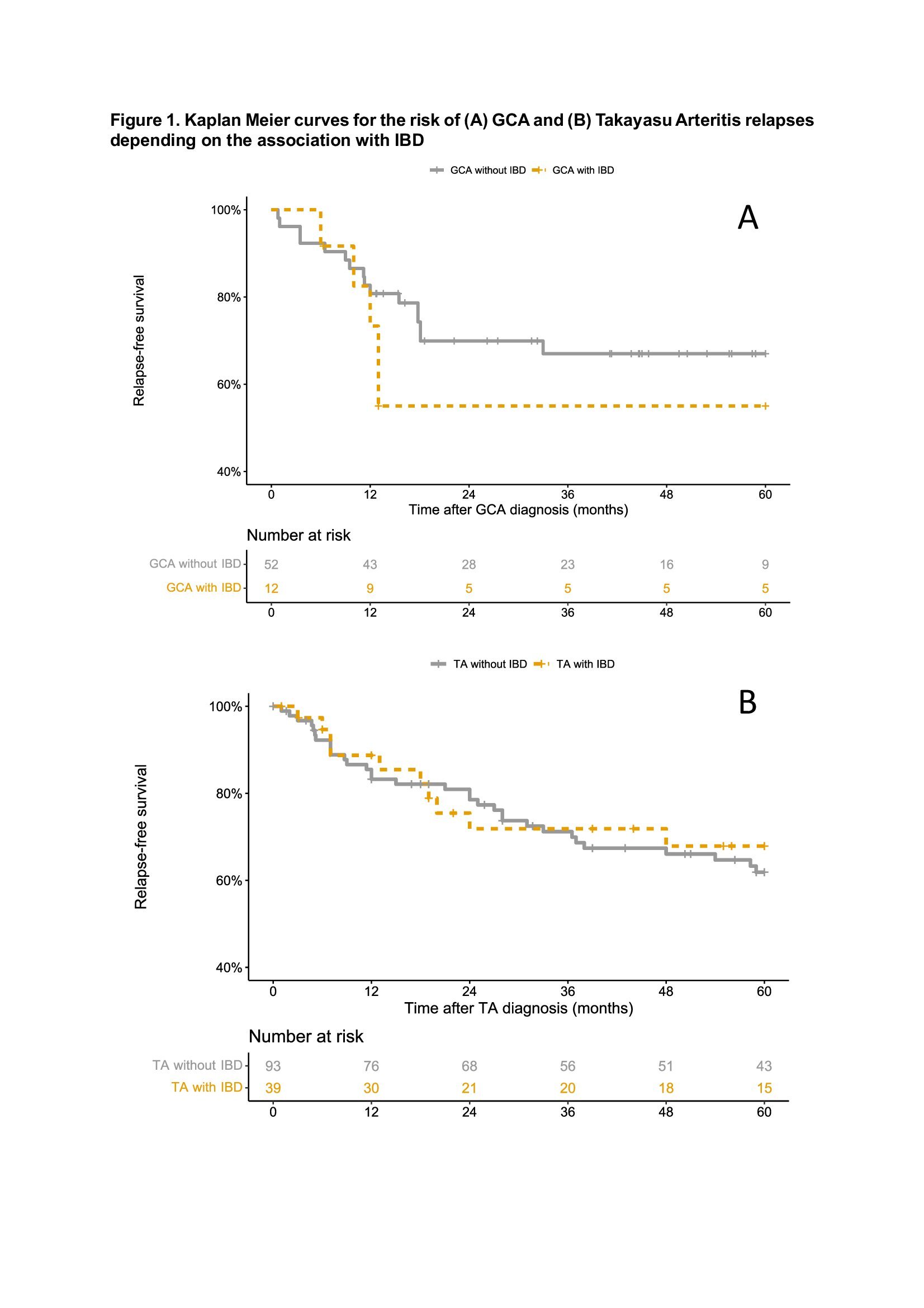
The presence of IBD did not influence the vasculitis relapse rate (OR 1.40 [0.39-5.10] for GCA and OR 0.72 [0.34-1.51] for TA). Aortic insufficiency in GCA patients (OR 8.36, 95% CI 1.35-51.66), and ascendent aorta involvement (OR 2.35, 95% CI 1.20-4.60) and the presence of general symptoms (HR 2.02, 95% CI 1.01-4.03) in TA patients were identified as independent vasculitis relapse risk factors.
Conclusion: This large case-control study identifies new clinical, imaging and outcome features in LVV-IBD. Vascular involvement seems to be less severe in TA-IBD than in iTA, while it seems to be the opposite in GCA-IBD. LVV-IBD occurred despite ongoing treatment in 77%, including AZA and/or TNF-a blockers in almost half of the cases.
To cite this abstract in AMA style:
Maillet F, Nguyen Y, Espitia O, Perard L, Salvarani C, Rivière E, Durel C, GUILPAIN P, Mouthon L, Kernder A, Loricera J, Cohen P, Melki I, De Moreuil C, Limal N, Mekinian A, Costedoat-Chalumeau N, Morel N, Boutemy J, Raffray L, Allain J, Devauchelle V, Kone-Paut I, Fabre M, Durel M, Dossier A, Abad S, Visentini M, Bigot A, Yildiz H, Fain O, Samson M, Gondran G, Abitbol V, Terrier B. Association of Large-vessel Vasculitis with Inflammatory Bowel Diseases: A European Case-control Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-of-large-vessel-vasculitis-with-inflammatory-bowel-diseases-a-european-case-control-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-large-vessel-vasculitis-with-inflammatory-bowel-diseases-a-european-case-control-study/