Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Giant cell arteritis (GCA) predominantly affects people over 50 years of age, with a female predominance. Its pathophysiological mechanism is currently under debate. In addition to genetic predisposition factors and a positive association between the onset of GCA with previous infections, there are some conflicting arguments for an association with cardiovascular risk factors.
Our aim was to determine whether cardiovascular risk factors are associated with the occurrence of GCA through a systematic literature review with meta-analysis.
Methods: Three authors independently performed a systematic review of Web of Science, PubMed and Embase up to 31 January 2024. PRISMA 2020 guidelines were applied. Studies were included if 1) their design was a case-control study, a cohort study or a cross-sectional study design; 2) the diagnosis of GCA was made by clinicians’ ascertainment, by ACR 1990 criteria, or by ICD-9,-10 code; 3) the diagnosis of a cardiovascular risk factor was based on clinician or biological ascertainment or on coding criteria. Studies with insufficient data to calculate an odds ratio (OR) or hazard ratio (95%CI) were excluded. The ROBINS-E tool (Risk Of Bias [ROB] In Non-randomized Studies – of Exposures) was used to assess bias. Studies assessing the same outcome were eligible for the quantitative analysis using Forrest plots to compare odds ratios (95%CI). The heterogeneity of studies was assessed using I2.
Results: A total of 4,210 citations were identified from the three databases. We excluded 957 duplicated articles and assessed 3,259 articles. A total of 23 studies were included in the qualitative synthesis and 21 in the meta-analysis, with a total of 15,305 GCA cases and 1,879,679 controls.
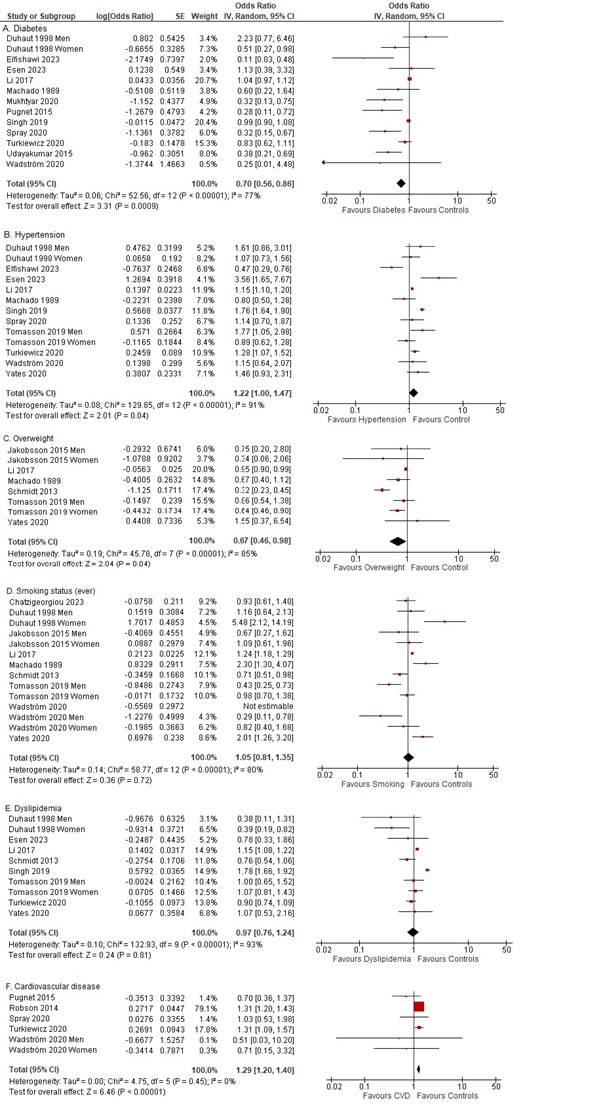
Twelve studies compared the incidence of GCA in patients with or without diabetes. In our meta-analysis, we found that diabetes was associated with a significant decrease of the risk of GCA (OR 0.70; 95% CI 0.56-0.86). (Figure 1) Similar trend was observed in our sensitivity analyses: when excluding studies with high ROB (OR 0.86; 95% CI 0.71-1.04) and when restricted to studies with ≥ 1 year between exposure and diagnosis of GCA (OR 0.37; 95% CI 0.10-1.41).
Compare to normal/low weight, overweight (defined as BMI > 25 kg/m2) was significantly associated with a decreased risk of incident GCA (OR 0.67; 95% 0.46-0.98). By contrast, hypertension was associated with a non-significant increased risk of subsequent GCA (OR 1.22; 95% CI 1.00-1.46).
No significant association was found with dyslipidemia (OR: 1.08, 95% CI 0.83-1.39) or smoking status (OR: 0.97, 95% CI 0.76-1.24). Finally, a personal history of cardiovascular disease was also found to significantly increase the risk of incident GCA (OR 1.2; 95% CI 1.20-1.40), but based on 5 studies with highly unbalanced weights.
Conclusion: This meta-analysis suggests that diabetes and overweight might have a protective effect on the risk of developing GCA, while hypertension tended to be associated with an increased risk of incident GCA.
Our study raises questions about the underlying mechanisms: association with cardiovascular risk factors themselves or with the use of specific medications.
Further prospective studies are needed to evaluate these hypotheses.
To cite this abstract in AMA style:
Barde F, Pacoureau L, Elbaz A, Seror R, Nguyen Y. Association Between Cardiovascular Risk Factors and the Onset of Giant Cell Arteritis: A Systematic Review and Meta-analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-between-cardiovascular-risk-factors-and-the-onset-of-giant-cell-arteritis-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-cardiovascular-risk-factors-and-the-onset-of-giant-cell-arteritis-a-systematic-review-and-meta-analysis/