Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Diffuse alveolar hemorrhage (DAH) is one of the most devastating complications of SLE. The exact pathogenesis leading to DAH in SLE is not well understood. Nonetheless, about a third of the patients with SLE have positive aPL, which are associated with non-thrombotic manifestations, including DAH. We aimed to assess the risk of DAH in patients with SLE based on their aPL profile by performing a systematic review (SR) and meta-analysis (MA).
Methods: MEDLINE, EMBASE, CENTRAL, and Scopus were systematically searched from inception to February 2023. Studies were eligible if they included SLE patients (population) with a description of the association of the aPL status (exposure) and DAH (outcome). SLE and DAH were defined as stated by the authors of primary studies. Studies were excluded if they reported findings only for patients with SLE with specific organ involvement. Two reviewers independently screened the studies and extracted data from the reports. The main analysis explored the association between any aPL (overall) and DAH; when multiple aPL subtypes were available in the same study, we prioritized their inclusion in the main analysis in the following order: 1) LA, 2) aCL, and 3) anti-β2 glycoprotein I (aβ2GPI). Subgroup analyses were performed by each aPL subtype. Sensitivity analyses assessed the effect of excluding studies where the population included only a subset of patients with SLE. Estimates were pooled using random-effects models, and the risk of bias was assessed using the Newcastle-Ottawa Scale. We followed the PRISMA guidelines for all stages of the SR and MA.
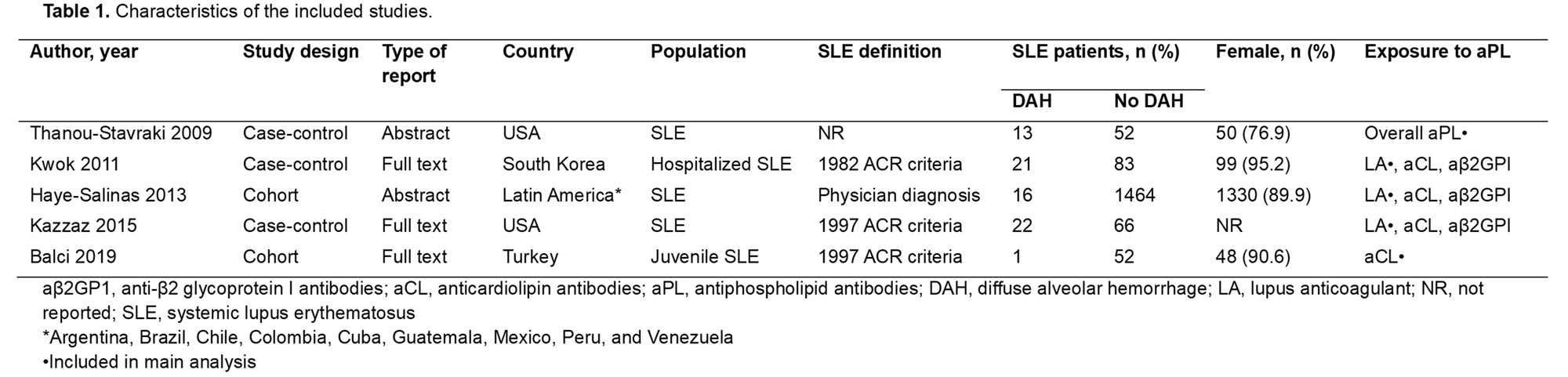
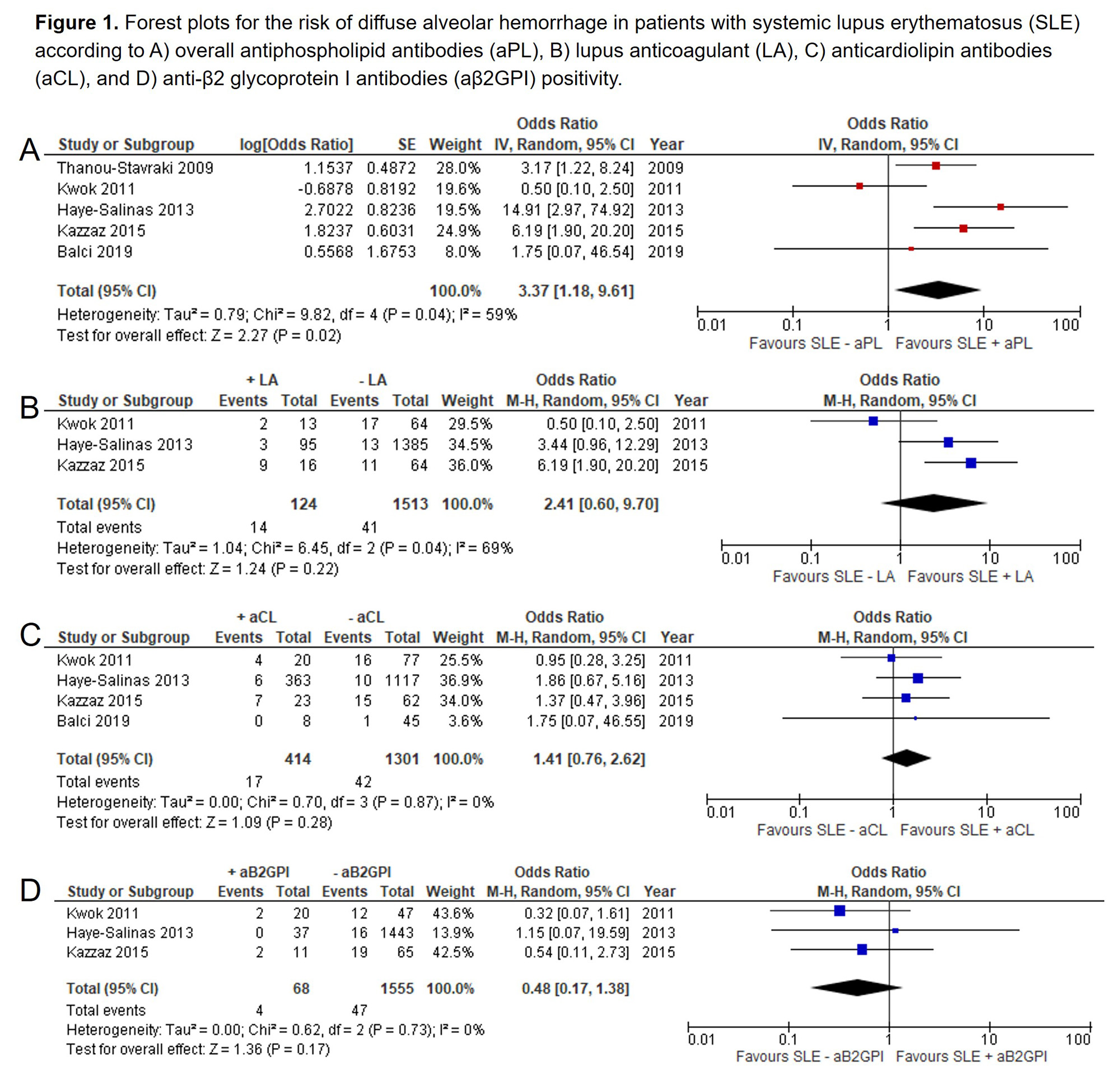
Results: A total of 399 studies were screened. Only five met inclusion criteria (three case-control and two cohort studies), adding up to 1790 patients with SLE and 73 events of DAH (Table 1). Patients with SLE and positive aPL (any) were three times more likely to have DAH than aPL-negative patients with SLE (OR 3.37, 95% CI 1.18-9.61; I2=59%; 1745 patients; 5 studies). Subgroup analyses based on aPL subtype showed that patients with SLE and positive LA (OR=2.41, 95% CI 0.60-9.70; I2=69%; 1637 patients, 3 studies), aCL (OR=1.41, 95% CI 0.76-2.62; I2=0%; 1715 patients; 4 studies), and aβ2GPI (OR=0.48, 95% CI 0.17-1.38; I2=0%; 1623 patients; 3 studies) had no significant difference in the risk of DAH compared to negative patients (Figure 1). Risk of bias assessment showed concerns in the definition and selection of the non-exposed participants and comparability between groups. Sensitivity analysis excluding studies with hospitalized SLE controls showed that patients with SLE and positive LA were four times more likely to present with DAH than negative patients (OR=4.72, 95% CI 1.98-11.22; I2=0%; 1560 patients; 2 studies).
Conclusion: In patients with SLE, aPL positivity might increase the risk of DAH compared with negative-aPL subjects. The certainty of our findings is limited by the paucity of available evidence exploring the aPL-DAH relationship, decreasing the precision of the risk assessment by aPL subtype.
To cite this abstract in AMA style:
Gonzalez-Trevino M, Yang J, Prokop L, Figueroa-Parra G, Duarte-Garcia A. Antiphospholipid Antibodies and the Risk of Diffuse Alveolar Hemorrhage in Patients with Systemic Lupus Erythematosus: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/antiphospholipid-antibodies-and-the-risk-of-diffuse-alveolar-hemorrhage-in-patients-with-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antiphospholipid-antibodies-and-the-risk-of-diffuse-alveolar-hemorrhage-in-patients-with-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/