Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Saturday, May 2, 2020
Title: Poster Session 3
Session Type: ACR Abstract Session
Session Time: 4:15PM-5:15PM
Background/Purpose: Lupus nephritis (LN) is related to disease severity, morbidity, and mortality in juvenile systemic lupus erythematosus (jSLE). Cluster analysis emerged to identify autoantibody profiles to better stratify disease phenotypes. Here, cluster analysis was performed to determine the existence of predictive autoantibody clusters in a cohort of biopsy-proven pediatric LN.
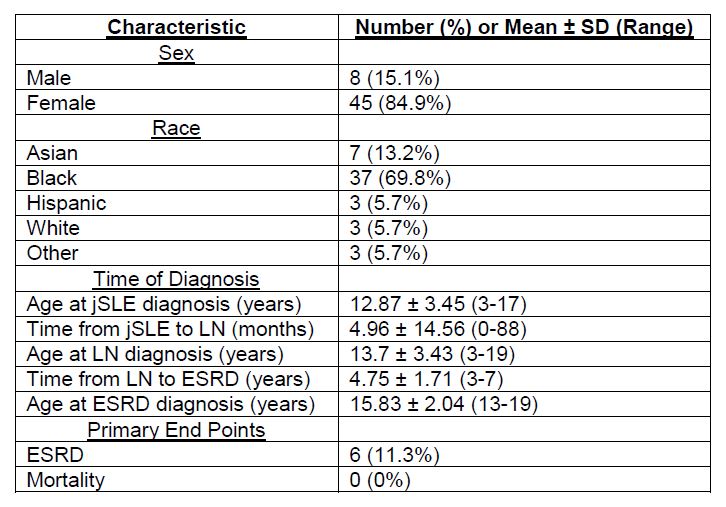
Methods: A retrospective chart review was performed of patients with jSLE found to have biopsy-confirmed LN at a quaternary pediatric hospital from 2007-2017. Primary endpoints: end-stage renal disease (ESRD) and mortality. K-medians clustering was performed, and patients with a complete autoantibody profile (ANA, anti-dsDNA, anti-Smith, anti-RNP, anti-Ro/SSA, anti-La/SSB) were included. Chi-square test was used for categorical variables. Kruskal-Wallis test was used for continuous measures. Significance was set at p< 0.05.
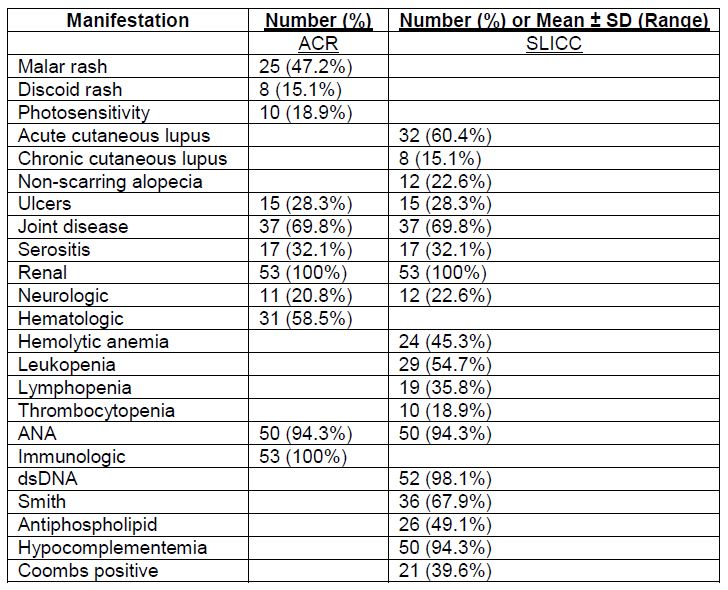
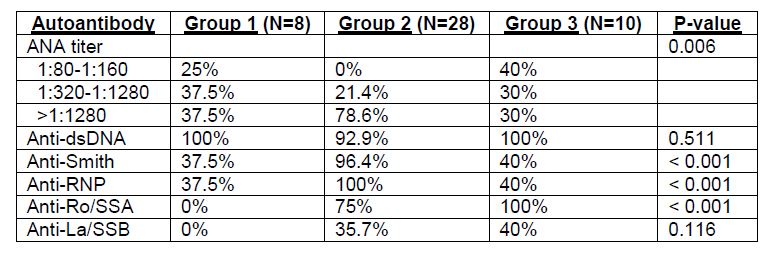
Results: Fifty-three patients met inclusion criteria. Demographics are listed in Table 1. Forty-nine (92.5%) fulfilled ACR and all (100%) fulfilled SLICC criteria based on biopsy-proven LN. jSLE manifestations are listed in Table 2. Most presented with LN within 1 year of jSLE (n=43, 81.1%), and LN was commonly the initial presentation (n=29, 54.7%). LN class V was most frequent (n=31, 58.5%) followed by class IV (n=28, 52.8%), class II (n=13, 24.5%), and class III (n=9, 17%). Twenty-two of those with LN class V and 3 of those with class IV were also positive for another class. Six progressed to ESRD. No mortalities were reported. ANA was positive in 94.3% of patients, of which 29 had titer >1:1280 (58%). Other autoantibody frequencies included: anti-dsDNA 96.2%, anti-RNP 67.9%, anti-Smith 66%, anti-Ro/SSA 62.3%, anti-La/SSB 26.4%. Forty-six had a complete autoantibody profile, including 4 with ESRD. Three distinct clusters were identified (Table 3). Anti-dsDNA was positive in all but one (97.8%). Group 1 was distinct by negative anti-Ro/SSA and anti-La/SSB; group 2 by predominantly high titer ANA ( >1:1280) and nearly all positive anti-Smith and anti-RNP; and group 3 by more commonly negative anti-Smith and anti-RNP and all positive anti-Ro/SSA. There was no significant difference in the distribution of sex, race, or jSLE manifestations. There was a significant difference in the distribution of LN class IV (p=0.016), with the highest percentage in group 1 (n=8, 100%) followed by group 3 (n=5, 50%) and group 2 (n=12, 42.9%). Those in group 3, significantly, were younger at diagnosis of jSLE (p=0.026) and LN (p=0.013), had higher creatinine (p=0.030) at LN diagnosis, and were more likely to progress to ESRD (p=0.025). All but 1 patient with ESRD was in cluster 3.
Conclusion: Cluster analysis revealed that in anti-dsDNA positive LN, the presence of anti-Ro/SSA is associated with earlier decline in renal function and increased risk for ESRD.
To cite this abstract in AMA style:
Sherman M, Gunawardana A, Amirault J, Moudgil A, Bost J, Srinivasalu H. Anti-Ro/SSA Is Associated with Progression to End-Stage Renal Disease in Anti-dsDNA Positive Lupus Nephritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/anti-ro-ssa-is-associated-with-progression-to-end-stage-renal-disease-in-anti-dsdna-positive-lupus-nephritis/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-ro-ssa-is-associated-with-progression-to-end-stage-renal-disease-in-anti-dsdna-positive-lupus-nephritis/