Session Information
Date: Tuesday, November 14, 2023
Title: (1945–1972) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Anti-PM/Scl autoantibodies (Abs) are an uncommon myositis-associated autoantibody (MAA) in juvenile myositis. The clinical features and outcomes associated with anti-PM/Scl Abs in juvenile myositis are largely uncharacterized.
Methods: Patients with juvenile myositis enrolled in NIH myositis natural history studies were screened for anti-PM/Scl and other myositis Abs. Demographics, clinical manifestations, medications, and outcomes of those with and without anti-PM/Scl Abs were compared using Chi-squared, Fisher’s exact test, or Wilcoxon rank-sum test. Multivariable logistic regression with adjustment for year of diagnosis and myositis autoantibodies was performed for statistically significant variables from the univariable analyses. A two-sided p< 0.05 was considered significant.
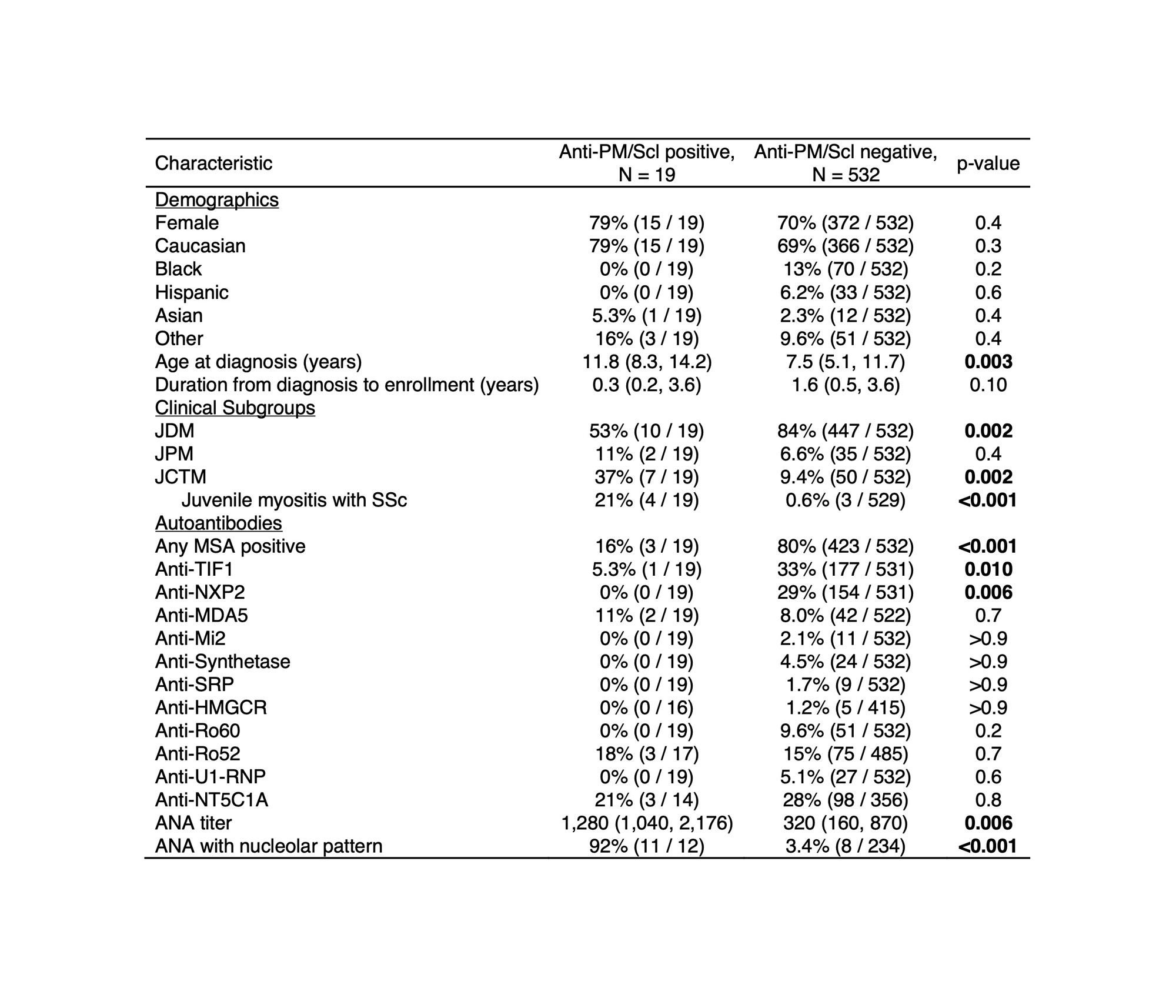
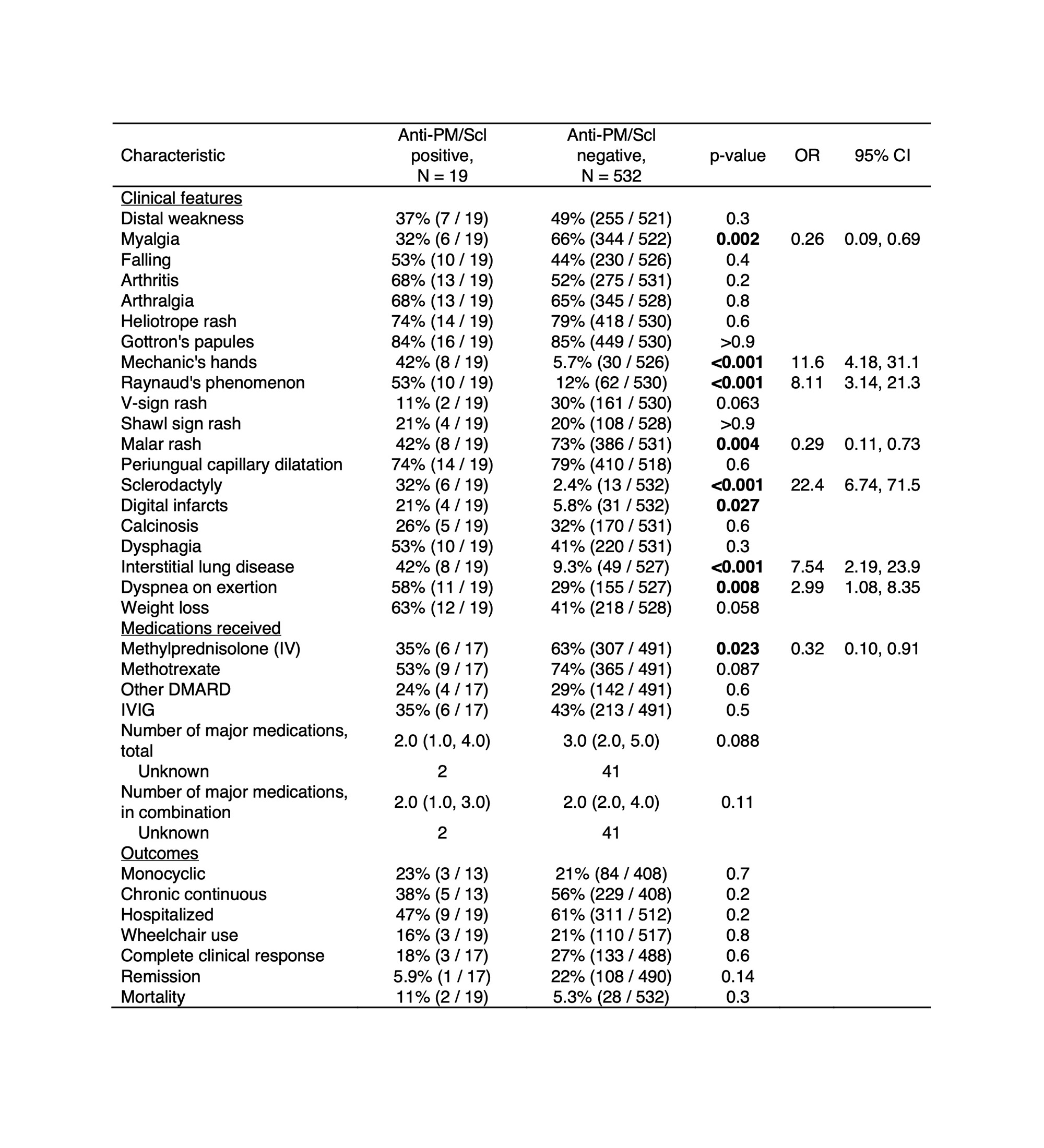
Results: Nineteen of 551 patients (3.4%) had anti-PM/Scl Abs by immunoprecipitation (Table 1). Among those with sera available for immunoblotting, 5 were positive for anti-PM/Scl-100, 1 was positive for anti-PM/Scl-75, 4 were positive for both antigens, and 3 were blot negative, likely reacting only to native protein. Patients with anti-PM/Scl Abs were older at diagnosis (11.8 vs 7.5 years, p=0.003) and more likely to have juvenile connective tissue disease myositis (37% vs 9.4%, p=0.002), frequently overlapping with systemic sclerosis (SSc) (21% vs 0.6%, p< 0.001). MSAs were less commonly associated with anti-PM/Scl Abs (16% vs 80%, p< 0.001). There was no difference in the frequency of anti-Ro52 Abs among patients with or without anti-PM/Scl Abs. ANA titer was higher (1:1280 vs 1:320, p=0.006) and a nucleolar pattern (92% vs 3.4%, p< 0.001) was more common among those with anti-PM/Scl Abs. Patients with anti-PM/Scl Abs had higher odds of certain clinical features (Table 2), including sclerodactyly (OR 22.4; 95% CI 6.74-71.5), mechanic’s hands (OR 11.6; 95% CI 4.18-31.1), Raynaud’s phenomenon (OR 8.11; 95% CI 3.14-21.3), and ILD (OR 7.54; 95% CI 2.19-23.9) and lower odds of malar rash (OR 0.29; 95% CI 0.11-0.73). There was also a lower odds of treatment with IV methylprednisolone (OR 0.32; 95% CI 0.10-0.91) for those with anti-PM/Scl Abs.
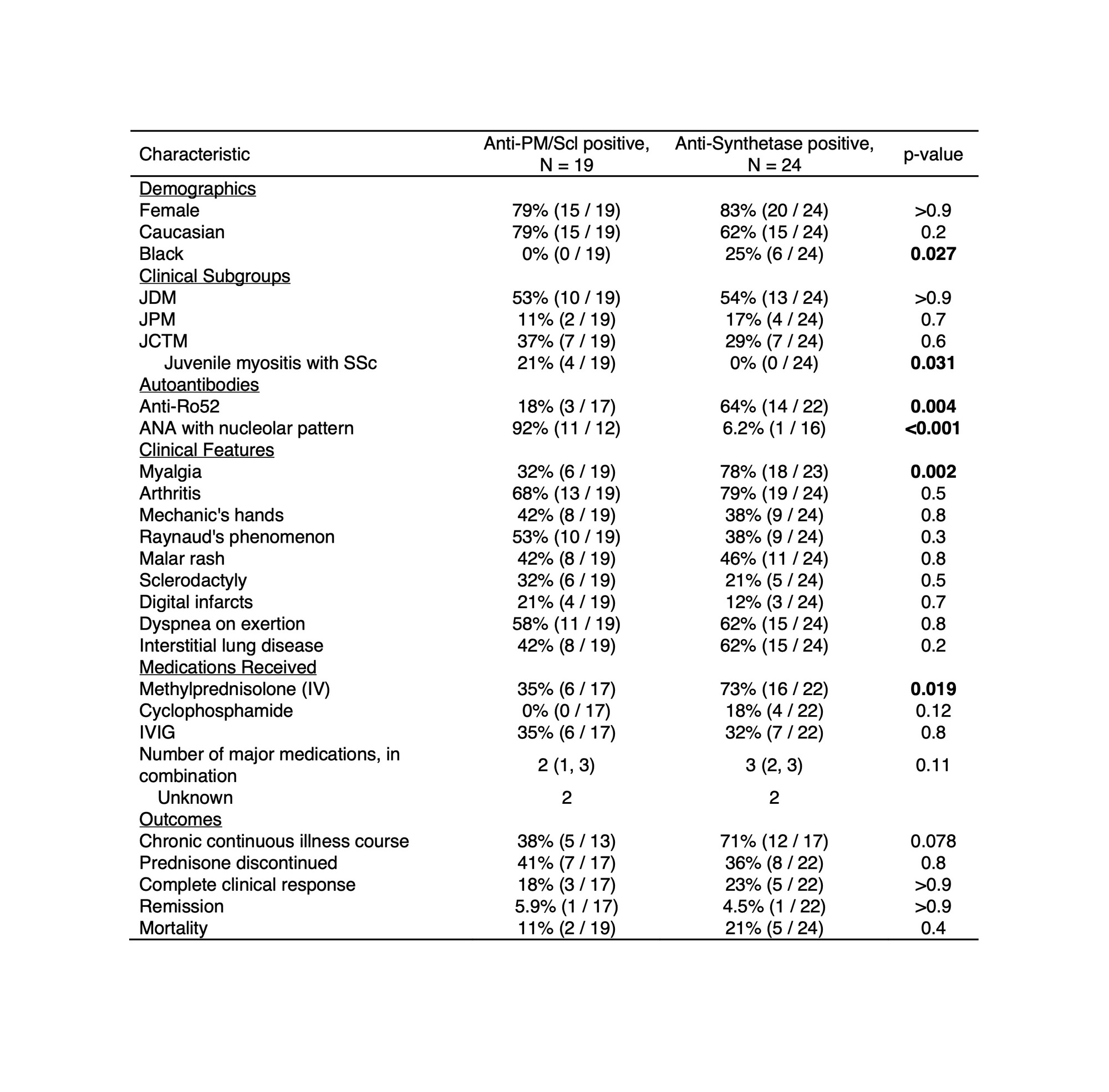
Given the similarity in clinical features to anti-synthetase syndrome, patients with anti-PM/Scl were compared to those with anti-aminoacyl tRNA synthetase (ARS) Abs (Table 3). Anti-ARS Abs were present in 24 (4.3%) patients, similar in frequency to anti-PM/Scl Abs. Among patients with anti-PM/Scl Abs, none was Black (0% vs 25%, p=0.027) and overlap with SSc was more common (21% vs 0%, p=0.031). Those with anti-PM/Scl Abs less often had co-occurring anti-Ro52 Abs (18% vs 64%, p=0.004) and myalgia (32% vs 78%, p=0.002). The presence of ANA with nucleolar pattern (92% vs 6.2%, p< 0.001) was more frequent in anti-PM/Scl Ab-positive patients.
Conclusion: Anti-PM/Scl Abs, unlike other MAAs, were associated with a well-defined phenotype resembling anti-synthetase syndrome. Patients with anti-PM/Scl Abs, compared to those with anti-ARS Abs, were not Black, had an ANA with nucleolar pattern, and less frequently were positive for anti-Ro52 Abs.
Acknowledgements: Intramural Research Program of NIAMS and NIEHS of the NIH.
To cite this abstract in AMA style:
Sherman M, Noroozi Farhad P, Trieu E, Pak K, Pinal-Fernandez I, Sarkar K, Neely M, Targoff I, Miller F, Mammen A, Rider L. Anti-PM/Scl Autoantibodies in Juvenile Myositis Are Associated with a Distinct Phenotype Resembling Anti-synthetase Syndrome [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/anti-pm-scl-autoantibodies-in-juvenile-myositis-are-associated-with-a-distinct-phenotype-resembling-anti-synthetase-syndrome/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-pm-scl-autoantibodies-in-juvenile-myositis-are-associated-with-a-distinct-phenotype-resembling-anti-synthetase-syndrome/