Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjögren’s disease (SjD) is an autoimmune disease characterized by a wide range of symptoms, and 30% to 60% of patients developed systemic manifestations. The most frequent autoantibodies are anti-SSA and anti-SSB antibodies, but others have been described, as anti-Ku antibodies. In patients with primary SjD (pSjD), whether anti-Ku antibodies are associated with a specific phenotype is unknown. Our study aimed to describe and compare the characteristics of patients with pSjD with and without anti-Ku antibodies.
Methods: All patients had to fulfill pSjD definition based on 2002 AECG or 2016 ACR/EULAR criteria. Patients with anti-Ku antibodies were screened through the database of the immunology departments of 6 tertiary university hospitals, and the recruitment is currently being extended. Patients without anti-Ku antibodies were recruited in a cohort of SjD patients participating to a multidisciplinary diagnostic session dedicated to SjD in a tertiary referral center. Patients with associated autoimmune disease were excluded.
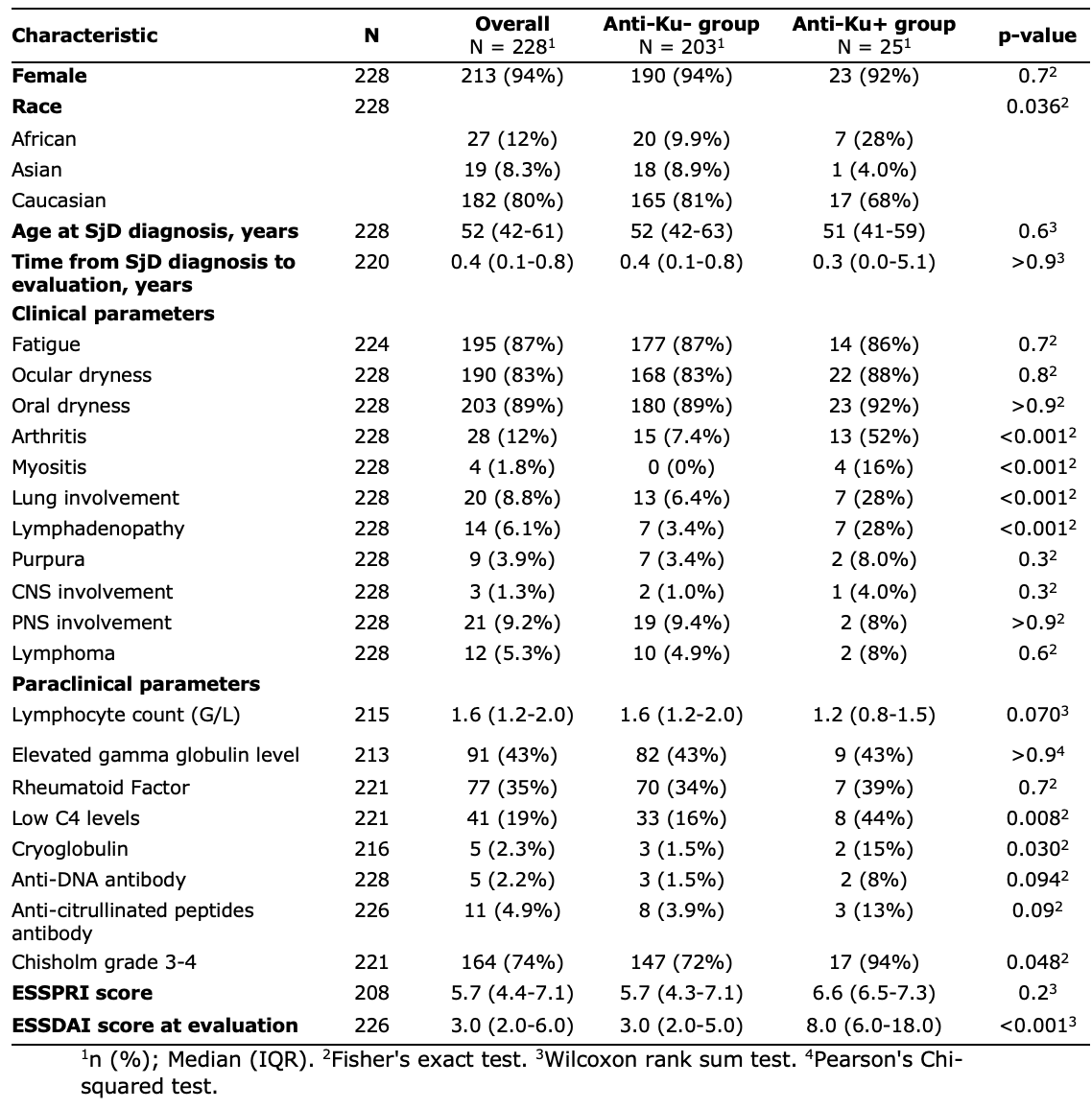
Results: Overall, 25 patients with pSjD positive for anti-Ku antibodies and 203 negative for anti-Ku antibodies were included. Sex-ratio, median age at diagnosis and the proportion of smokers were similar between groups. There was a higher proportion of patients of African ancestry in the anti-Ku+ group (28% vs 9.9%). The median time between diagnosis and the evaluation was not different between groups (Table 1). At evaluation, patients with anti-Ku antibodies displayed more frequently lymphadenopathies and arthritis compared with anti-Ku negative patients (28% vs 3.4%. p< 0.001; 52% vs 7.4%. p< 0.001). The proportions of patients with lung involvement and myositis were significantly higher in anti-Ku positive group (28% vs 6.4%, p< 0.01 and 16% vs 0%, p< 0.001 respectively). Pain, fatigue and dryness were comparable between groups. Biological (i.e., lymphocyte count, gammaglobulin level) features were similar between groups, except for cryoglobulinemia which was more frequent in patients with anti-Ku antibodies (15% vs 1.5%, p=0.03). Anti-citrullinated peptides, anti-SSB, anti-RNP, anti-dsDNA antibodies and rheumatoid factor were found in similar proportions whereas anti-SSA were less frequent in anti-Ku+ patients (36% vs 71%, p< 0.001). Median ESSDAI was significantly higher in anti-Ku + group compared with anti-Ku- (8.0 [6.0-18.0] vs 3.0 [2.0-5.0], p< 0.001). The occurrence of lymphoma was not different between groups (2 patient in anti-Ku+ group [8.0%], 10 patients in anti-Ku- group [4.9%], p=0.6) (Table 1).
Conclusion: pSjD patients with anti-Ku antibodies displayed a more active systemic disease than patients without anti-Ku antibodies. Lung and muscle involvement should be carefully monitored in these patients.
To cite this abstract in AMA style:
ROBERT M, Nguyen Y, Uzunhan Y, Terrier B, Allenbach Y, Meyer A, Gottenberg J, HADJADJ J, Amoura Z, HOT A, Bettacchioli E, Aslangul E, Belkhir R, Desmoulins F, Bergé E, Chrétien P, Roland-Nicaise P, Goulvestre C, Charuel J, Nespola B, Fabien N, Ballot E, Nocturne G, Mariette X, Bitoun S, Seror R. Anti-Ku Positivity in Primary Sjögren’s Disease Is Associated with a More Systemic Active Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anti-ku-positivity-in-primary-sjogrens-disease-is-associated-with-a-more-systemic-active-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-ku-positivity-in-primary-sjogrens-disease-is-associated-with-a-more-systemic-active-disease/