Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Heat shock protein 90 alpha (HSP90α) is an epichaperone present ubiquitously inside the cell, whose dimers function as a foldase that helps the correct assemble of client proteins. In a mouse model of systemic lupus erythematosus (SLE), increased expression of HSP90α has been observed in kidney sections, and its blocking has demonstrated protective effects in regards to proteinuria and autoantibody production. In patients with SLE, increased sera levels of HSP90α have been suggested to correlate with clinical activity. Antibodies (Ab) against HSP90α have been detected in healthy individuals, without any apparent pathological effect, being thus categorized as “natural antibodies”. Here we describe, for the first time, a potential protective role of anti-HSP90α Ab in decreasing the risk of secondary antiphospholipid syndrome (APS) in patients with SLE.
Methods: Presence of anti-HSP90α IgG was evaluated in plasma samples from SLE patients, and population controls (PC) from two independent cohorts, by means of an in-house immunoassay (ELISA). The exploratory cohort was comprised by 306 SLE individuals (29 with concomitant APS), paired with 306 PC, from the Karolinska Institutet SLE cohort. The validation cohort was represented by 125 SLE individuals (14 with concomitant APS), and 77 PC, from the Lund University Biobank. In vitro studies were performed with platelets from healthy donors incubated with mitochondria isolated from HepG2 cells. Mitochondria, abundant sources of HSP90, were treated with IgG-free sera in addition to either an anti-HSP90α Ab or an isotype control. Detection of platelet activation markers thrombospondin-1 (TSP-1) and platelet factor-4 (PF-4) in supernatant was evaluated by ELISA.
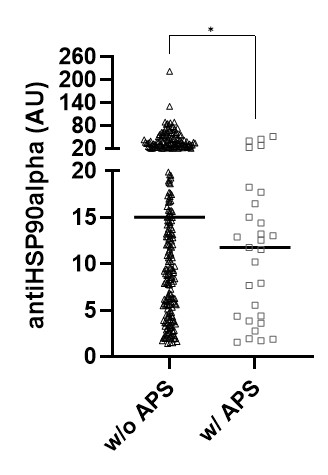
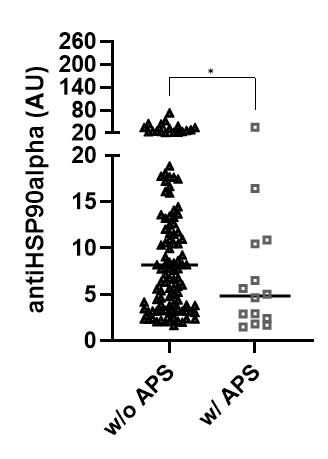
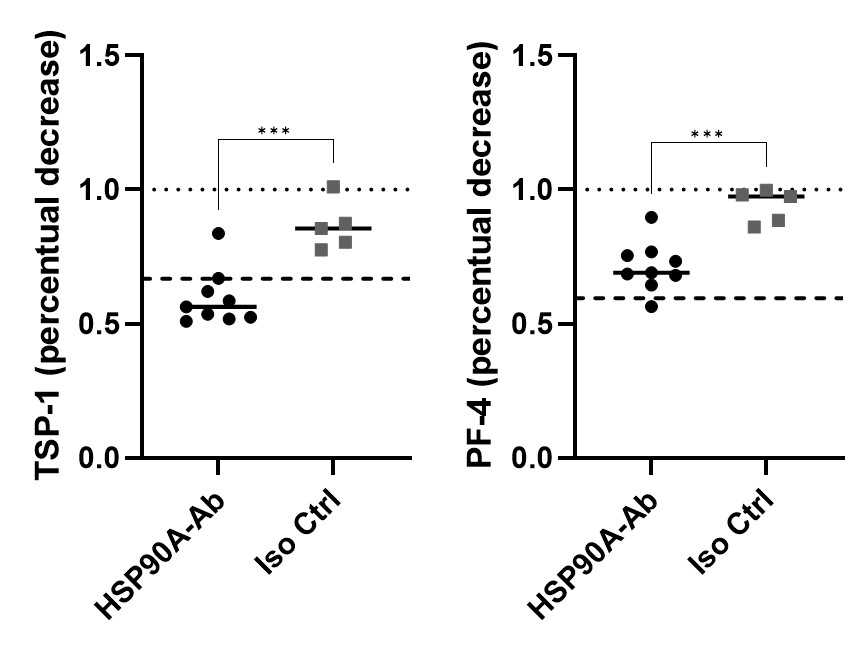
Results: Anti-HSP90α IgG was detected similarly in SLE and PC, with no difference in mean values, in both cohorts. However, after stratifying data for clinical features and outcomes, we observed that SLE patients with APS presented significantly reduced titers (expressed in arbitrary unit – AU) of the antibody as compared to those without APS (11.8 AU vs. 15.0 AU, p = 0.0265, in the Karolinska cohort; and 4.8 AU vs. 8.2 AU, p = 0.0472, in the Lund cohort). To confirm the biological relevance of these findings, we evaluated the capacity of anti-HSP90α Ab to decrease platelet activation, assessing secretion of TSP-1 and PF-4. When co-cultured with mitochondria pre-treated with IgG-free sera, platelets secrete high amounts of TSP-1 and PF-4 as compared to non-stimulated platelets (mean 10.2 ug/mL vs. 6.9 ug/mL, and mean 491 ng/mL vs. 293 ng/mL, respectively). By pre-treating mitochondria with anti-HSP90α Ab, the increase of those markers was significantly reduced, the same not happening when adding an isotype control (for TSP-1: 7.3 ug/mL vs. 8.9 ug/mL, respectively; for PF-4: 321 ng/mL vs. 449 ng/mL, respectively).
Conclusion: Our study is the first to demonstrate an inverse association between presence of anti-HSP90α IgG and risk of APS in SLE. We propose that this antibody may block the recognition of HSP90 by platelets, and thus diminish platelet activation and, ultimately, thrombosis.
To cite this abstract in AMA style:
Barguil Macedo M, Gonzalez-Chapa J, Bengtsson A, Gunnarsson I, Svenungsson E, Lood C. Anti-HSP90α as a Protective Natural Antibody Against Secondary Antiphospholipid Syndrome in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anti-hsp90%ce%b1-as-a-protective-natural-antibody-against-secondary-antiphospholipid-syndrome-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-hsp90%ce%b1-as-a-protective-natural-antibody-against-secondary-antiphospholipid-syndrome-in-systemic-lupus-erythematosus/