Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a disease characterized by the presence of auto-antibodies, immune complex deposition, and a robust type 1 interferon signature. It is widely known that SLE patients often have Coombs positivity, suggesting the presence of anti-erythrocyte antibodies. The presence of these antibodies in the absence of hemolytic anemia have long been thought to be clinically insignificant, though an association with a more severe disease phenotype has been reported. Recent work in pediatric SLE has implicated anti-erythrocyte antibodies in disease pathogenesis via opsonization of mitochondria-containing erythrocytes, leading to enhanced erythrophagocytosis and induction of type-1 interferon production by myeloid cells (Caielli et al., 2021). Still, little is known about anti-erythrocyte antibodies in pediatric SLE, including their prevalence, association with disease activity and phenotype, and antigenic target or specificity. The primary objective of this project is to confirm the presence of anti-erythrocyte antibodies in pediatric SLE patients. Additional objectives include characterization of the target antigens and functional properties of these antibodies, as well as to correlate their presence with disease activity and phenotype.
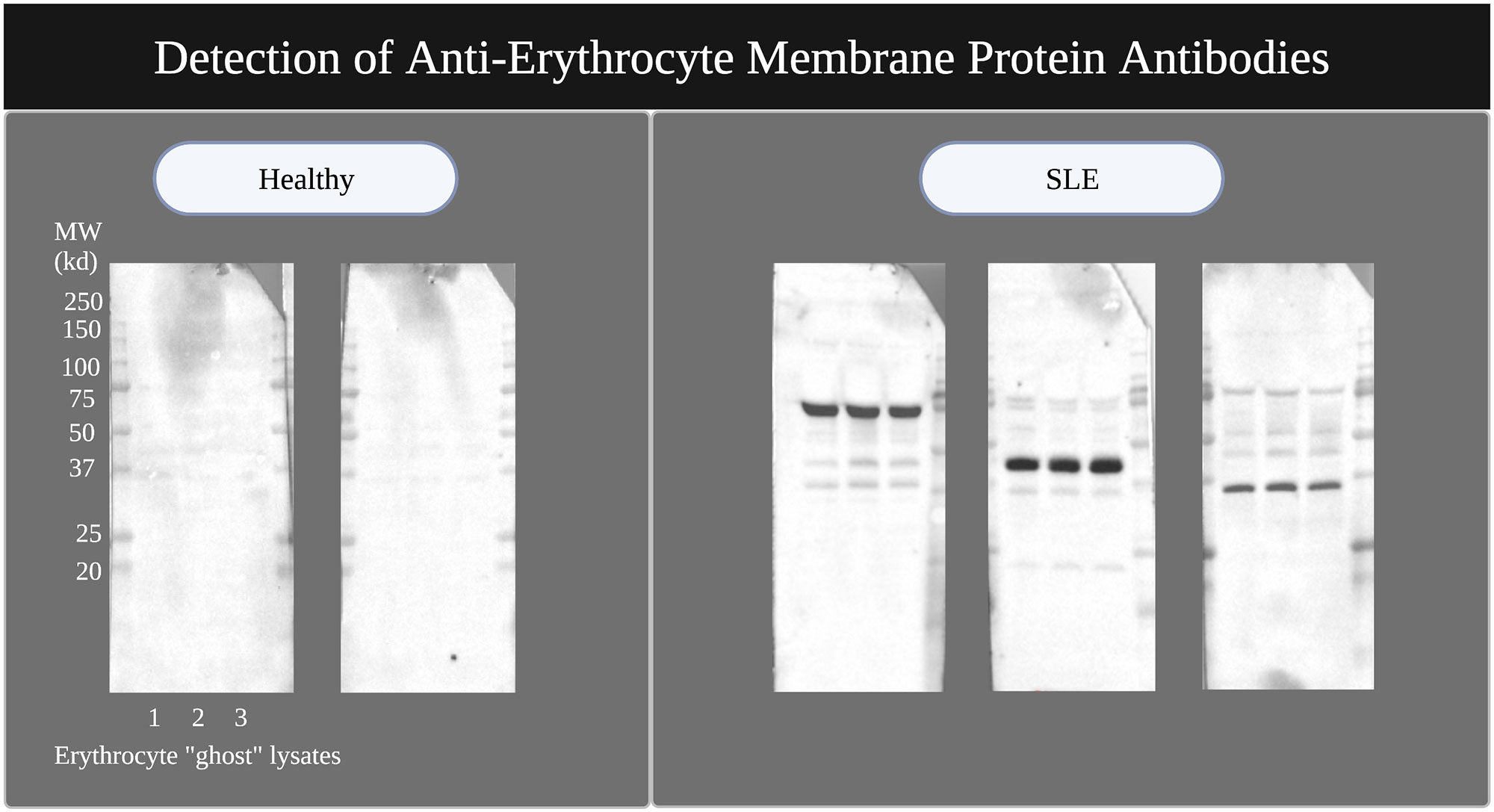
Methods: Serum from 8 pediatric healthy controls and 20 pediatric SLE patients was analyzed for detection of anti-erythrocyte membrane protein antibodies. Erythrocyte membrane protein lysate was generated via the creation of erythrocyte “ghost” membranes and used as a substrate for western blotting. Membranes with erythrocyte membrane proteins were probed with healthy serum or pediatric SLE serum, and the presence of IgG against erythrocyte membrane protein was revealed with anti-human IgG conjugated to HRP.
Results: 15 of 20 pediatric SLE serum samples had strongly positive IgG bands to erythrocyte protein antigens on western blot, compared to 0 of 8 healthy pediatric controls. The SLE serum samples showed reactivity against several target antigens of different molecular weights ranging from 25-250kd, and patterns of reactivity varied between samples [Figure 1]. The most prevalent immunoreactive band was at a molecular weight of 75kd (7 of 20 pediatric SLE samples). There was no correlation between the presence of anti-erythrocyte antibodies and hemoglobin or hematocrit.
Conclusion: This study supports the presence of anti-erythrocyte antibodies in a majority of patients with pediatric SLE in the absence of anemia. Future studies will focus on identifying the target erythrocyte proteins and establishing whether a correlation exists between these antibodies and the capacity to opsonize and enhance erythrophagocytosis in vitro. Our ultimate goal is to determine the role these antibodies may play in disease pathogenesis.
To cite this abstract in AMA style:
Robinson L, Wan Z, Balasubramanian P, Rodriguez Alcazar J, Walters L, Baisch J, onel k, Wright T, Pascual V, Caielli S. Anti-Erythrocyte Antibodies in Childhood Onset Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/anti-erythrocyte-antibodies-in-childhood-onset-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-erythrocyte-antibodies-in-childhood-onset-systemic-lupus-erythematosus/