Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The overall mortality rate in ankylosing spondylitis (AS) patients is increased by 60–90% compared with the general population. This higher mortality rate is predominately caused by cardiovascular disease (CVD) comprising an increased prevalence of cardiac diseases such as valvular heart disease, conduction disturbances and cardiomyopathies as well as atherosclerotic diseases such as myocardial infarctions. However, there is a lack of contemporary studies. Therefore, we investigated current prevalences of cardiac disorders in a well characterized cohort of Dutch patients with AS compared to osteoarthritis (OA) controls.
Methods: We performed a cross-sectional study in AS and OA patients between 50-75 years. Subjects were recruited from a large rheumatology outpatient clinic (Reade) in Amsterdam, the Netherlands. Patients underwent echocardiography with 2D, spectral and Color Doppler imaging. The echocardiogram was evaluated by an experienced and certified cardiologist. Diastolic dysfunction was assessed according to the ASE/EACVI 2016 guideline. Furthermore, blood sample, surveys and physical examination were done. Disease activity and function were measured with the BASFI, BASDAI and the ASDAS-CRP.
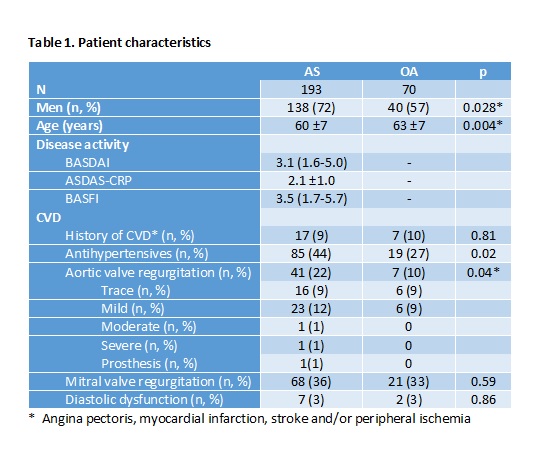
Results: A total of 193 consecutive AS patients were included with a median age of 60 (±7) years of which 72% men (138). The control group consisted of 70 OA patients (table 1). In the AS cohort the disease activity measures , BASDAI, ASDAS-CRP and BASFI, indicated moderate disease activity and were, respectively 3.1 (1.6-5.0), 2.1 (±1.0) and 3.5 (1.7-5.7). Anti-TNF was used by 43% of the AS patients. History of cardiovascular disease (CVD), i.e. angina pectoris, myocardial infarction, stroke and/or peripheral ischemia was comparable between the AS and OA cohort, respectively 9% (17) and 10% (7), p=0.81. Antihypertensives were significantly more often used in AS patients, 85 (44%) vs 19 (27%), p=0.02. Prevalences of systolic dysfunction and diastolic dysfunction did not differ significantly in AS and OA patients, respectively 6 (5%) vs 2 (5%), p=0.96 in systolic dysfunction and 7 (3%) vs 2 (3%), p=0.86 in diastolic dysfunction. Prevalence of aortic valve (AV) regurgitation was significantly higher in AS patients compared to OA patients, respectively 41 (22%) and 7 (10%), mostly with mild severity. The prevalence of mitral valve (MV) regurgitation did not differ between the AS and OA patients, respectively 68 (36%) vs 21 (33%), p=0.59. When corrected for age, gender and cardiovascular risk factors in a regression analysis, AS patients still had a substantially increased risk for AV regurgitation, odds ratio (OR) 2.8 95%CI 1.1-7.2, p=0.038.
Conclusion: This study demonstrates an almost tripled risk for developing AV regurgitation in Dutch AS patients. Although mostly mild in this age, due to the progressive nature of AV regurgitation in AS, echocardiographic screening should be considered in elderly AS patients.
To cite this abstract in AMA style:
Baniaamam M, Heslinga S, Boekel L, Handoko M, Konings T, Kamp O, van Halm V, van Denderen J, van der Horst-Bruinsma I, Nurmohamed M. Ankylosing Spondylitis Patients at Risk of Developing Aortic Valve Regurgitation, Need for Mandatory Echocardiography? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/ankylosing-spondylitis-patients-at-risk-of-developing-aortic-valve-regurgitation-need-for-mandatory-echocardiography/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ankylosing-spondylitis-patients-at-risk-of-developing-aortic-valve-regurgitation-need-for-mandatory-echocardiography/