Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Tracheobronchial disease is a common manifestation of ANCA associated vasculitis (AAV). However, outcomes data is commonly unreported in prospective studies. We performed a retrospective review to evaluate the relapse rate of large airway disease on common immunosuppression regimens.
Methods: A retrospective review was conducted on patients with diagnosis of AAV who had undergone evaluation for tracheobronchial disease between 01/01/2002 and 9/6/2022 at a Mayo Clinic site. Patients under the age of 18 or those who lacked follow-up extending to 6 months or longer were excluded. Differences between groups were tested using equal variance two sample t-tests or Fisher’s exact tests. Sensitivity and specificity with exact binominal confidence intervals were calculated for unique baseline symptoms for prediction of large airway involvement.
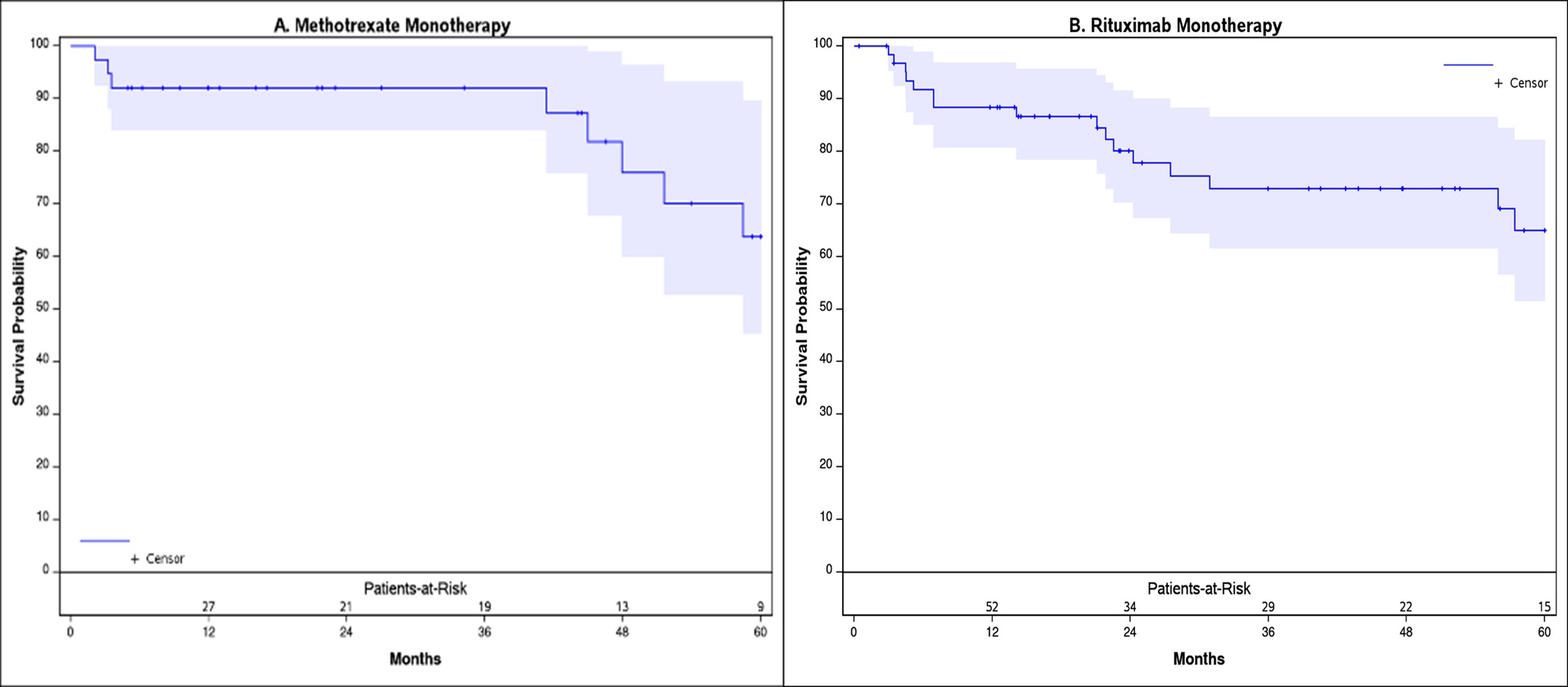
Time to relapse of the airway disease, as defined by persistent inflammation with or without progressive narrowing, was estimated using the Kaplan-Meier method for methotrexate and rituximab monotherapy. Patients were censored at treatment end, start of new therapy, or last follow-up. Time to relapse was analyzed at the patient-period level.
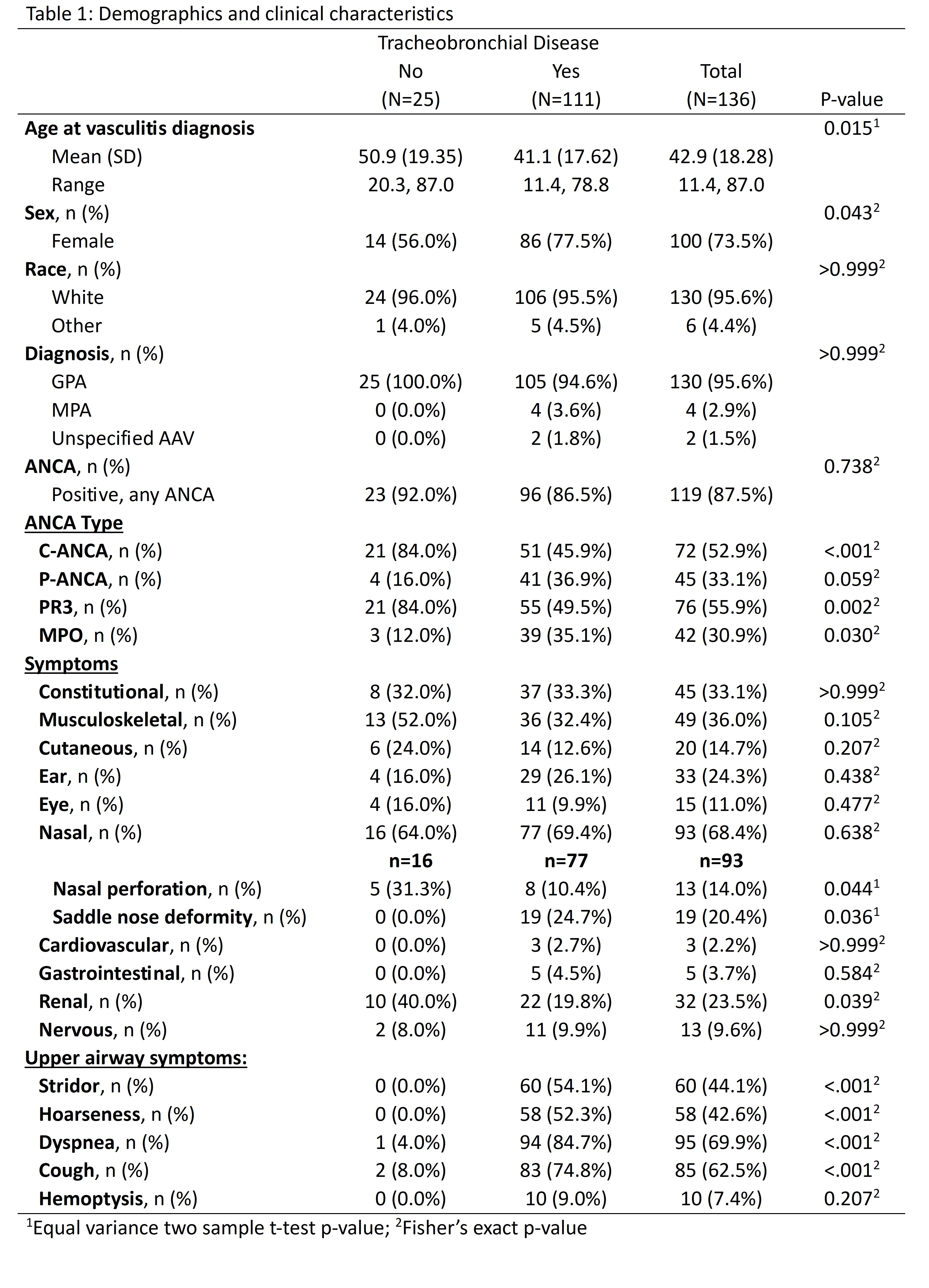
Results: One hundred thirty-six patients with AAV who had undergone assessment for tracheobronchial involvement were included. 111 (81.6%) patients had tracheobronchial involvement. Younger age (Mean 41.1 vs 50.9, p = 0.015) and female gender (77.5% vs 56.0%, p = 0.043) were associated with large airway involvement. MPO positivity is represented more frequently in the large airway group (12% vs 35.1%, p = 0.030). Renal disease was inversely associated (40% vs 19.8, p = 0.039). Saddle nose deformity occurred more often in those with tracheobronchial disease that had nasal manifestations (0/16 [0%] vs 19/77 [24.7%], p = 0.036). Stridor and hoarseness were common symptoms among patients with large airway disease (0% vs 54.1% and 0% vs 52.3%, p < 0.001). Pooled sensitivity for the combined variable of hoarseness and stridor was 74.77 (95% CI 65.65-82.54) with specificity at 100 (95% CI 86.28-100.00).
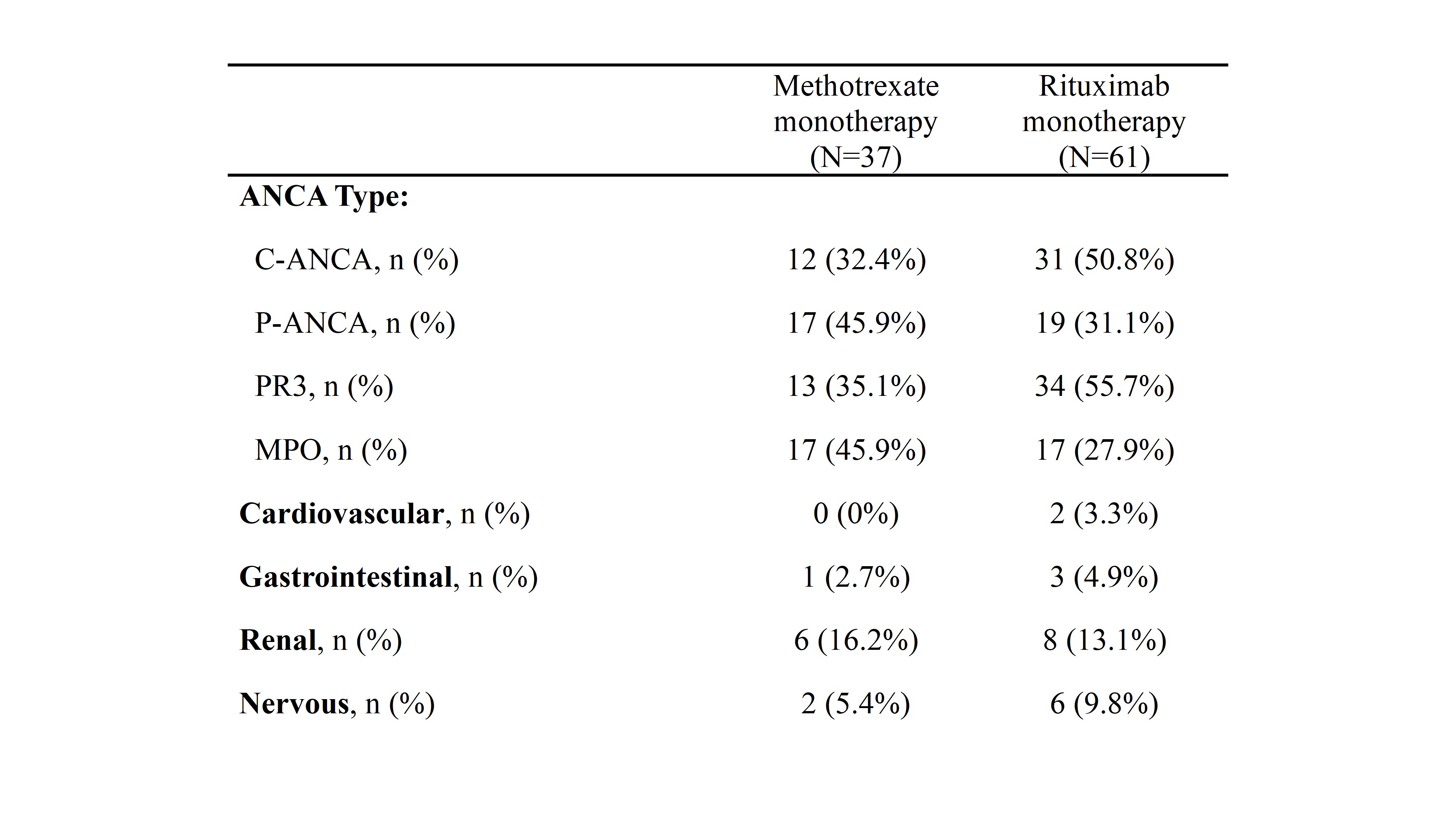
66 (59.5%) had undergone localized treatment with endoscopic dilation or injection. There were 63 patient-periods of rituximab monotherapy and 38 patient-periods of methotrexate monotherapy. Baseline characteristics are listed in Table 2. The 12-month progression free survival time estimate for rituximab was 88.4% (CI 80.7-96.9) and 92.1% (CI 83.9-100.0) for methotrexate (Figure 1). 60-month survival time estimates were 65.0% (CI 51.5-82.1) and 63.7% (CI 45.3-89.7), respectively.
Conclusion: Younger age, female gender, and saddle nose deformity were positively associated with development of tracheobronchial disease in our ANCA vasculitis cohort. Renal involvement had an inverse association. The presence of hoarseness or stridor was very specific for tracheobronchial disease. Of patients with a diagnosis of AAV-associated tracheobronchial disease, 5-year relapse rates were high, even while on immunosuppression with methotrexate or rituximab. There is an unmet need for adequate treatment regimens of this common manifestation.
To cite this abstract in AMA style:
Sullivan M, Diaz Menindez M, Butendieck R, baig h, Irani A, Wang B, Berianu F, Mead-Harvey C, Abril A, Majithia V. ANCA Associated Tracheobronchial Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anca-associated-tracheobronchial-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anca-associated-tracheobronchial-disease/