Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Large pediatric rheumatology centers receive hundreds of yearly referrals with a wide variety of complaints and diagnoses. The amount of referrals received can lead to long appointment wait times and delayed diagnosis of rheumatic conditions. In this study, we analyze three years of new patient referrals as the first step toward improving the quality of outpatient referrals and promptness of rheumatic disease diagnosis.
Methods: All patients referred to the University of Alabama at Birmingham Pediatric Rheumatology clinic between January 2019 and December 2021 were identified. Referral and discharge diagnoses and scheduled follow up appointments were abstracted from the electronic medical record. Per clinic policy, all referrals under 18 years of age were offered an appointment, regardless of concern for rheumatic disease. Descriptive data are presented as average and percentages. The analysis excludes hospital follow-up patients that were seen as new clinic patients. This study is exempt from Institutional Review Board review as data was obtained and analyzed for quality improvement purposes.
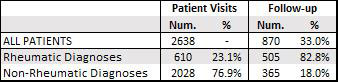
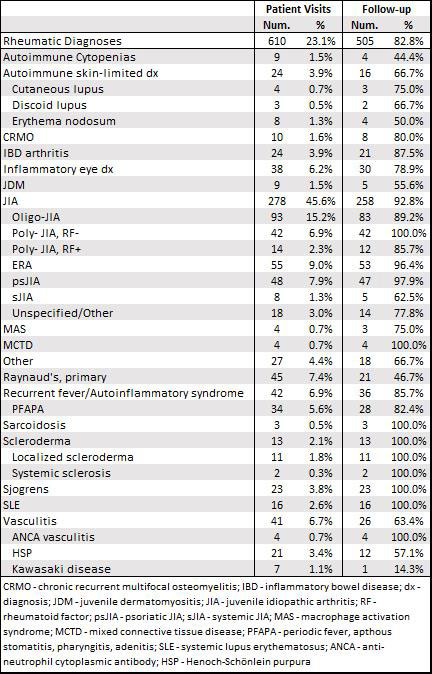
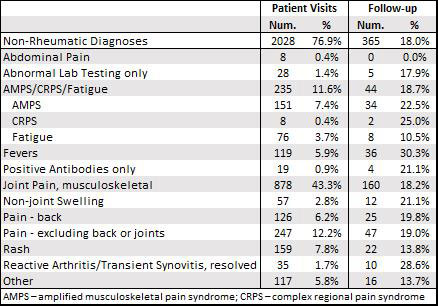
Results: During the study period, 2638 new patients were referred to the University of Alabama at Birmingham Pediatric Rheumatology clinic. On average, 73 new patients were referred per month, with monthly referrals peaking at 137 visits in March 2021 and reaching their nadir – 30 and 31 referrals in March and April 2020, respectively – due to restricted in-person visits at the onset of COVID-19 protocols. Of the total referred patients, 610 (23.1%) were diagnosed with a rheumatic condition during their initial or follow-up appointments. Juvenile idiopathic arthritis (JIA) was the most frequent diagnosis at 45.6% of patients, including oligoarticular JIA and enthesitis-related JIA at 15.2% and 9.0% of patients respectively. The next most common diagnoses were primary Raynaud’s phenomenon at 7.4%, recurrent fever or autoinflammatory syndromes at 6.9%, vasculitides at 6.7%, and inflammatory eye conditions at 6.2%. Inflammatory bowel disease arthropathy, Sjogren’s syndrome, systemic lupus erythematosus, and juvenile dermatomyositis each made up less than 5% of total diagnoses. Non-rheumatic diagnoses totaled 76.9% (2028 pts) of referrals. Pain was the most common non-rheumatic diagnosis, with musculoskeletal joint pain (878 patients, 43.3%), back pain (126, 6.2%), and extremity/muscle pain (247, 12.2%) together representing over half of all referred patients. Amplified musculoskeletal pain syndrome, complex regional pain syndrome, and chronic fatigue collectively made up 11.6% of non-rheumatic diagnoses, with rash and fevers following at 7.8% and 5.9% respectively. Only 33% of all referred patients were ever seen for a follow-up visit, including 82.8% of rheumatic diagnoses and 18% of non- rheumatic diagnoses.
Conclusion: The vast majority of patients referred to our pediatric rheumatology clinic do not have a rheumatic disorder and do not follow-up beyond their initial appointment. Strategies to ensure individuals with rheumatic disease receive a timely diagnosis by pediatric rheumatologists will become more important with worsening workforce shortages.
To cite this abstract in AMA style:
Reiff D, Mannion M, Smitherman E, Stoll M, Weiser P, Cron R. Analysis of New Patient Referrals to a Large Pediatric Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/analysis-of-new-patient-referrals-to-a-large-pediatric-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-new-patient-referrals-to-a-large-pediatric-rheumatology-clinic/