Session Information
Date: Sunday, October 26, 2025
Title: (0337–0356) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoporosis is under screened in men. The United States Preventive Services Task Force (USPSTF) does not publish guidelines for osteoporosis screening in men. Other professional societies only recommend screening when certain risk factors are present. The Fracture Risk Assessment Tool cites risk factors including rheumatoid arthritis (RA), smoking, alcohol use, glucocorticoid use, and family history of hip fracture. In addition to RA, literature evidence links low bone mineral density to autoimmune connective tissue disease (CTD) and seronegative spondyloarthropathy (SpA) 1. Our study assesses provider recognition of rheumatic disease as a risk for osteoporosis by examining the prevalence of dual-energy X-ray absorptiometry (DXA) screening in men with rheumatic disease. We hypothesized that osteoporosis is under screened among men with rheumatic diseases.
Methods: We conducted a retrospective cohort study using electronic health record data from the Stony Brook system from 1/1/2000 to 12/15/2024. We identified 38,970 men with current age 50 and older with ICD-10 codes mapped to RA, SpA, osteoarthritis (OA), polymyalgia rheumatica (PMR), crystal arthropathy (CA), vasculitis, and CTD. Osteoporosis screening was defined as at least one CPT code corresponding to a DXA scan after initial documentation of a disease or risk factor. We performed bivariate logistic regression to assess the unadjusted association between DXA screening and disease groups, smoking, family history of osteoporosis, alcohol abuse/dependence, long-term systemic steroid use, and demographics. Variables meeting a relaxed Wald p ≤ 0.2 were included in a multivariate logistic regression model to identify independent predictors of screening.
Results: The percentage of patients with DXA was low in all disease cohorts, with an average screening rate of 4.05%. The highest rates were seen in PMR (8.33%) and RA (5.10%) and the lowest in CA (1.59%). The yield of osteoporosis among those screened ranged from 20.95% (CTD) to 41.91% (SpA) with the average yield being 31.51% (Figure 1). Increasing age, long-term steroid use, RA, PMR, SpA, and CTD were all significantly associated with DXA screening (Figure 2).
Conclusion: Providers screened patients with autoimmune diseases in greater percentages than patients with OA or CA, and autoimmune diseases except vasculitis were significantly associated with DXA screening. Long-term steroid use was the only significant non-disease predictor of DXA screening. One limitation is the undefined duration of “long-term” use in the associated ICD-10 code, though chronicity is implied. Family history of osteoporosis was excluded; its wide confidence interval (OR 7.6, 95% CI 1.7–33.3) reflects low documentation, likely during DXA referrals, limiting its reliability as an independent predictor. Despite low screening rates, the yield of osteoporosis among screened patients was substantial. With growing recognition of autoimmunity as an osteoporosis risk factor, we are optimistic that more patients will receive timely diagnosis and treatment. 1. Bultink, I.E.M. et al. Inflammatory Rheumatic Disorders and Bone. Curr Rheumatol Rep 14, 224–230 (2012). doi.org/10.1007/s11926-012-0252-8
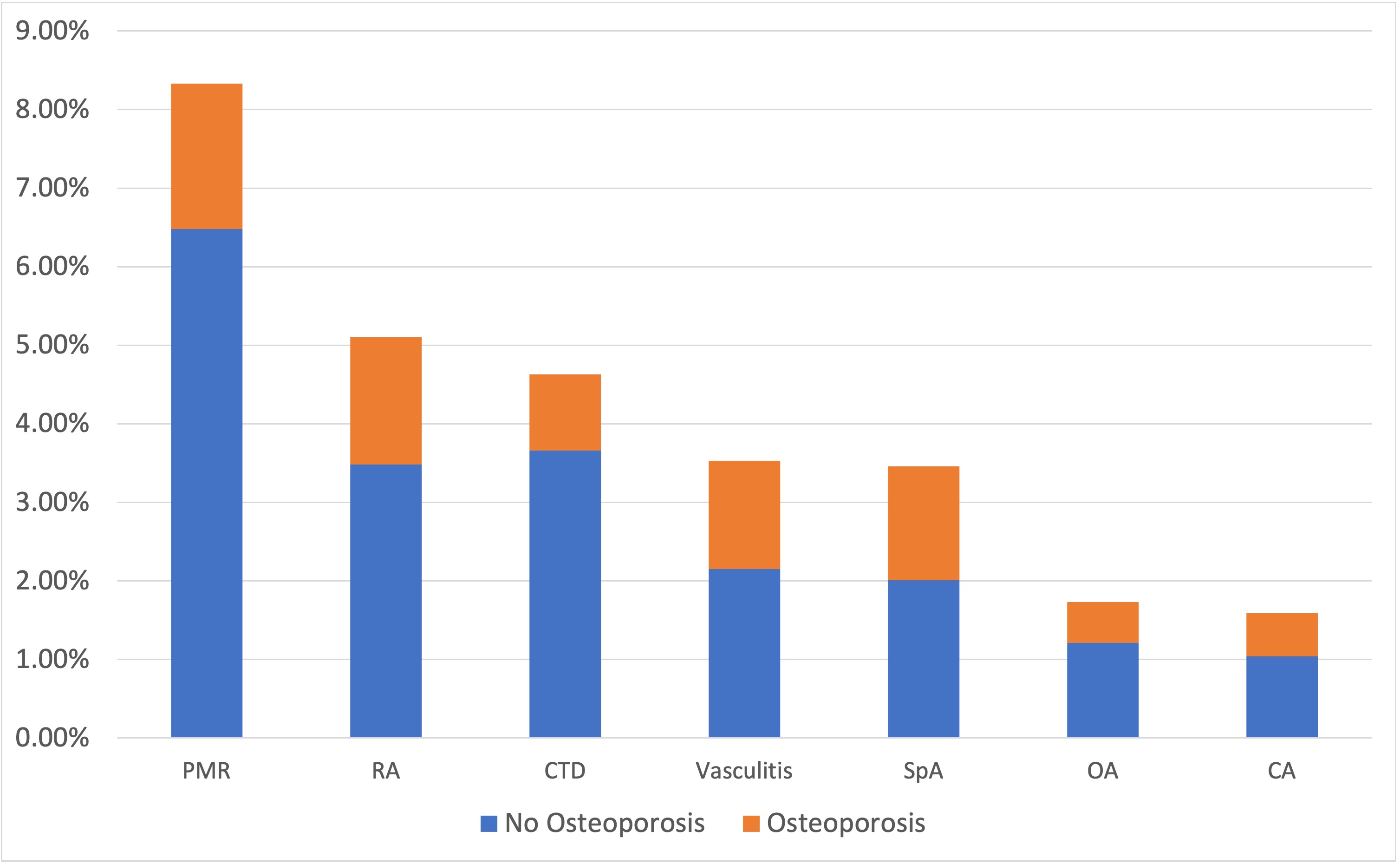 Figure 1. Total percentage of screened patients within each disease cohort, along with the percentage of those patients found to have osteoporosis.
Figure 1. Total percentage of screened patients within each disease cohort, along with the percentage of those patients found to have osteoporosis.
.jpg) Figure 2.Variables meeting a relaxed Wald p ≤ 0.2 in bivariate logistic regression with the outcome of DXA screening were included in a multivariate logistic regression model. The resulting odds ratios and confidence intervals are displayed in this forest plot.
Figure 2.Variables meeting a relaxed Wald p ≤ 0.2 in bivariate logistic regression with the outcome of DXA screening were included in a multivariate logistic regression model. The resulting odds ratios and confidence intervals are displayed in this forest plot.
To cite this abstract in AMA style:
Poos S, Nguyen H, Greenberg S, Lee M, Roppelt H, Patnaik A. An Analysis of Osteoporosis Screening in Males 50 and Older with Rheumatic Disease across Stony Brook Medicine Network [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/an-analysis-of-osteoporosis-screening-in-males-50-and-older-with-rheumatic-disease-across-stony-brook-medicine-network/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-analysis-of-osteoporosis-screening-in-males-50-and-older-with-rheumatic-disease-across-stony-brook-medicine-network/
