Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Rheumatoid arthritis (RA) is a chronic inflammatory joint disease with episodic flares. In tumor necrosis factor transgenic (TNF-Tg) mice, a model of inflammatory-erosive arthritis, the popliteal lymph node (PLN) enlarges during the pre-arthritic “expanding” phase, and then “collapses” with adjacent knee flare associated with the loss of the intrinsic lymphatic pulse. Thus, a critical question is whether loss of the lymphatic pulse can be recovered by standard RA therapies.
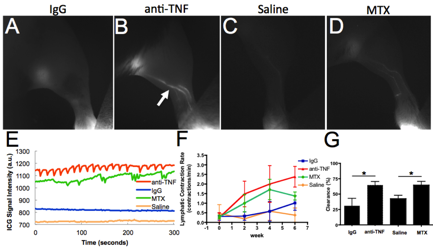
Methods: We tested the hypothesis that anti-TNF vs. irrelevant IgG (IgG); and methotrexate (MTX) vs. saline treatment ameliorates knee synovitis adjacent to collapsed PLN in TNF-Tg mice by restoring the lymphatic pulse using contrast enhancement MRI (CE-MRI), ultrasound, near infrared indocyanine green (NIR-ICG) imaging, transmission electron microscopy (TEM) and flow cytometry.
Results: Anti-TNF treatment significantly decreased normalized synovial volume compared to IgG (0.87±0.21 vs. 1.52±0.16; p<0.05), measured by CE-MRI. This decrease correlated with a lower power Doppler volume within the joint, a measure of inflammation, in both anti-TNF and MTX treated mice compared to placebo treated (0.04±0.01 vs. 0.20±0.03 mm3 and 0.05±0.01 vs. 0.18±0.08 mm3, respectively; p<0.05). Lymphatic pulse rate and clearance were measured via NIR-ICG imaging (Figure). As predicted, anti-TNF significantly increased the lymphatic pulse vs. IgG (2.63±0.68 vs. 0.99±0.36 pulses/min), and MTX also induced an increase vs. saline (1.38±0.21 vs. 0.38±0.38 pulses/min), although this effect was weaker than anti-TNF. Consistently, footpad clearance of ICG was higher in anti-TNF and MTX treated mice vs. placebos (64.53±6.08 vs. 30.84±12.26 and 64.54±6.20 vs. 42.49±5.69, respectively; p<0.05). To gain insight into the mechanism of lymphatic pulse restoration, TEM was performed on the lymphatic vessels. We found that placebo treated mice showed damaged lymphatic endothelial cells (LECs) and smooth muscle cells (LSMCs), while anti-TNF treated mice showed intact LECs and LSMCs apical to fibrotic tissue, suggestive of tissue repair. Interestingly, anti-TNF treatment resulted in a significant ~4-fold increase in monocyte numbers normalized to placebo vs. MTX (3.77±0.77 vs. 1.08±0.19 cells per PLN; p<0.05), via flow cytometry. We previously reported monocytes trafficking in afferent lymphatic vessels. Thus, these findings indicate increased transit of monocytes to the PLN from the inflamed joint.
Conclusion: These NIR-ICG, CE-MRI and flow cytometry results demonstrate that anti-TNF increases lymphatic transport to a greater extent than MTX. Furthermore, our data suggest that the primary mechanism for monocyte (type 1 synoviocyte) removal from inflamed joints following anti-TNF treatment is through restoration of lymphatic pulse and cellular egress.
Disclosure:
E. M. Bouta,
None;
I. Kuzin,
None;
K. de Mesy-Bentley,
None;
R. Wood,
None;
H. Rahimi,
None;
R. C. Ji,
None;
C. T. Ritchlin,
Eli Lilly and Company,
9,
Eli Lilly and Company,
5;
A. Bottaro,
None;
L. Xing,
None;
E. M. Schwarz,
Johnson & Johnson,
5,
NIAMS-NIH,
2.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/amelioration-of-inflammatory-arthritis-by-anti-tnf-therapy-is-associated-with-restoration-of-lymphatic-contraction/