Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Arthritis of the temporomandibular joint, or TMJ arthritis, is an underrecognized manifestation of juvenile idiopathic arthritis (JIA). The absence of prompt treatment may lead to orofacial symptoms, dysfunction, and permanent deformities. Little is known about the education that adult and pediatric rheumatology fellows receive about TMJ arthritis. In this survey-based study, program directors were queried about the education that their trainees receive about TMJ arthritis in patients with JIA.
Methods: We conducted an electronic-based survey study of adult and pediatric rheumatology program directors (ARPDs and PRPDs, respectively) in the United States and Canada. The survey was sent via REDCap at intermittent intervals from November 2023 to March 2024. Responses were collected anonymously, and descriptive statistics were performed using Stata 15.1.
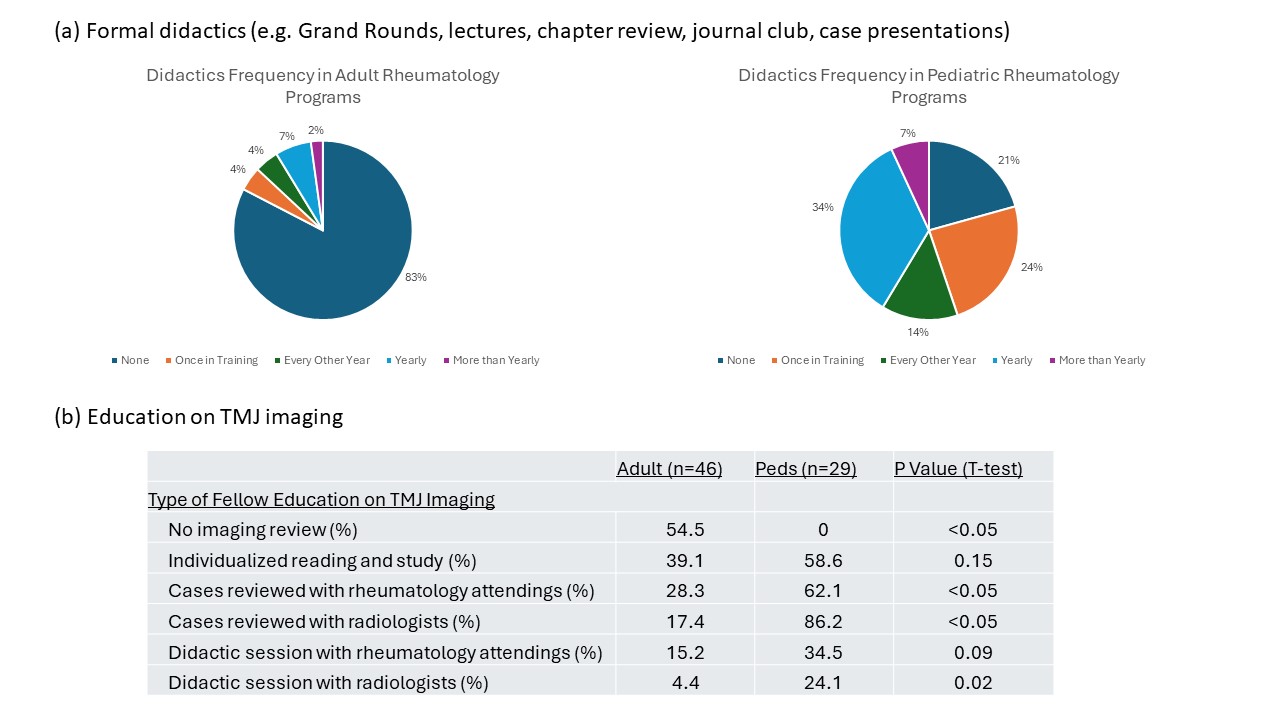
Results: Survey response rate was 72.5% among PRPDs (29/40) and 33.1% among ARPDs (46/139). Respondents represented all regions of the U.S. and parts of Canada (Table 1). PRPDs reported having 0-7 fellows (median = 3, interquartile range (IQR) = 1-4). ARPDs reported having 0-10 fellows (median = 4, IQR = 3-6). There were 0-3 Med-Peds fellows at each program. 100% (29/29) of PRPDs and 78.2% (36/46) of ARPDs reported that their fellows had clinical exposure to patients with JIA who have TMJ arthritis (Fisher’s exact, p< 0.05). 4.6% (n=3) of programs had dedicated TMJ arthritis clinics, all of which included oral maxillary facial specialists (OMFS) and dentists. While 23 of 29 (79.3%) pediatric programs held formal didactics on TMJ arthritis, only 8 of 46 (17.4%) adult programs did (Fisher’s exact, p< 0.001, Fig. 1). Among both adult and pediatric programs, in addition to rheumatologists and rheumatology trainees, radiologists (9%), OMFS (7%), dentists and/or orthodontists (1%), and therapists (1%) attended these formal didactics. Fellow education on TMJ arthritis imaging was much more often performed in pediatric as opposed to adult rheumatology programs (100% vs. 45.5%, T-test, p< 0.05; Fig. 1).
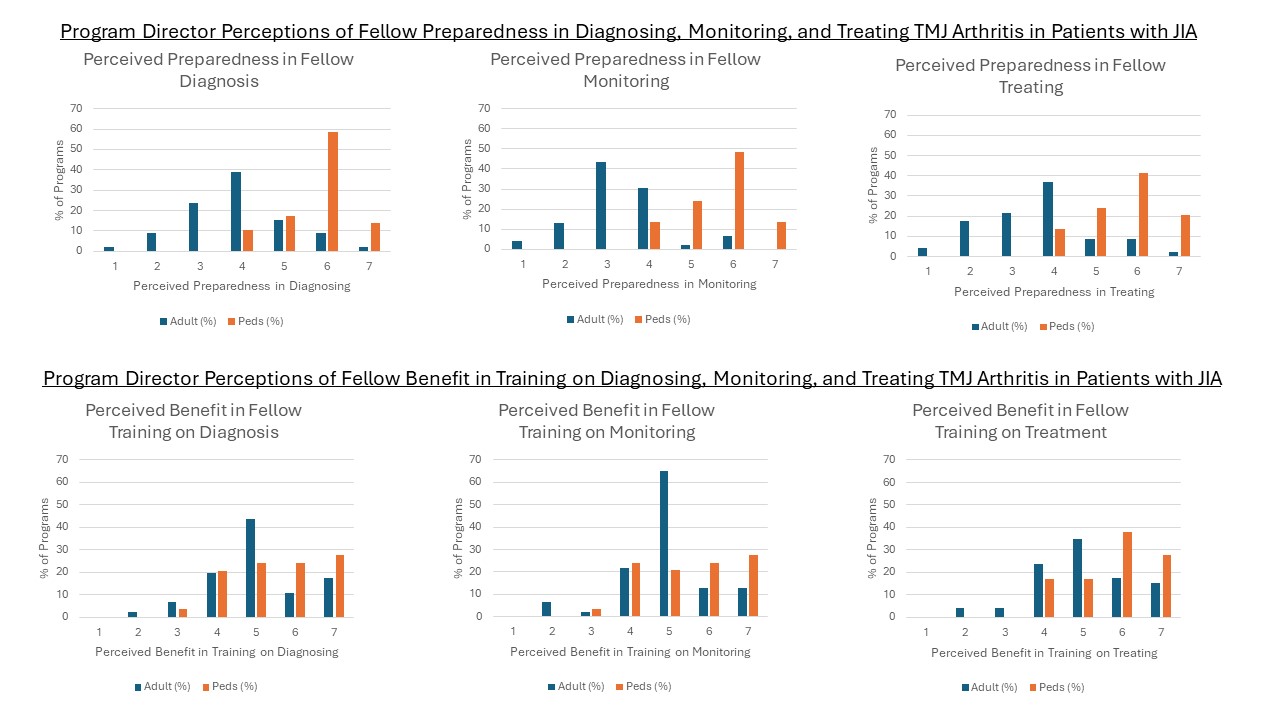
There were significant differences reported by ARPDs vs. PRPDs in their perception of the level of preparedness of their graduating fellows to diagnose, monitor, and treat TMJ arthritis (each p=0.0001, Kruskal-Wallis; Fig. 2), as well as the perceived benefit of additional training in treating TMJ arthritis (p=0.0136, Kruskal-Wallis; Fig. 2). Among adult programs, there was an association between the presence of fellows’ clinical exposure to patients with JIA who have TMJ arthritis and the perceived level of preparedness in diagnosing (chi2, p=0.018) and treating (chi2, p=0.029) TMJ arthritis in these patients, but not the perceived level of monitoring it. There were no associations between adult fellows’ clinical exposure to patients with JIA who have TMJ arthritis and the perceived level of benefit to having more training in diagnosing, monitoring, or treating TMJ arthritis in patients with JIA.
Conclusion: This study provides insights into the differences in education that adult and pediatric rheumatology fellows receive on TMJ arthritis in patients with JIA. These data can be used to inform educational initiatives on TMJ arthritis for trainees.
To cite this abstract in AMA style:
Bayefsky S, Ryan M, Pan N, Ronis T, Twilt M, Lerman M, TMJ Workgroup C. Adult and Pediatric Rheumatology Fellow Education on Temporomandibular Joint (TMJ) Arthritis in Patients with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/adult-and-pediatric-rheumatology-fellow-education-on-temporomandibular-joint-tmj-arthritis-in-patients-with-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adult-and-pediatric-rheumatology-fellow-education-on-temporomandibular-joint-tmj-arthritis-in-patients-with-juvenile-idiopathic-arthritis/