Session Information
Date: Monday, November 8, 2021
Session Type: Abstract Session
Session Time: 9:45AM-10:00AM
Background/Purpose: SLE is a chronic autoimmune disease driven by immune dysregulation. We have previously identified patterns of disordered immunity present prior to and concurrent with the accrual of SLE-associated autoantibodies (AutoAbs) and classification criteria (Munroe et al. Ann Rheum Dis. 2016; Lu et al. J. Autoimmun. 2016). This study seeks to determine the feasibility of an immune mediator-informed Lupus Classification Risk Immune Index (LCRII) to distinguish patients who transition to classified SLE.
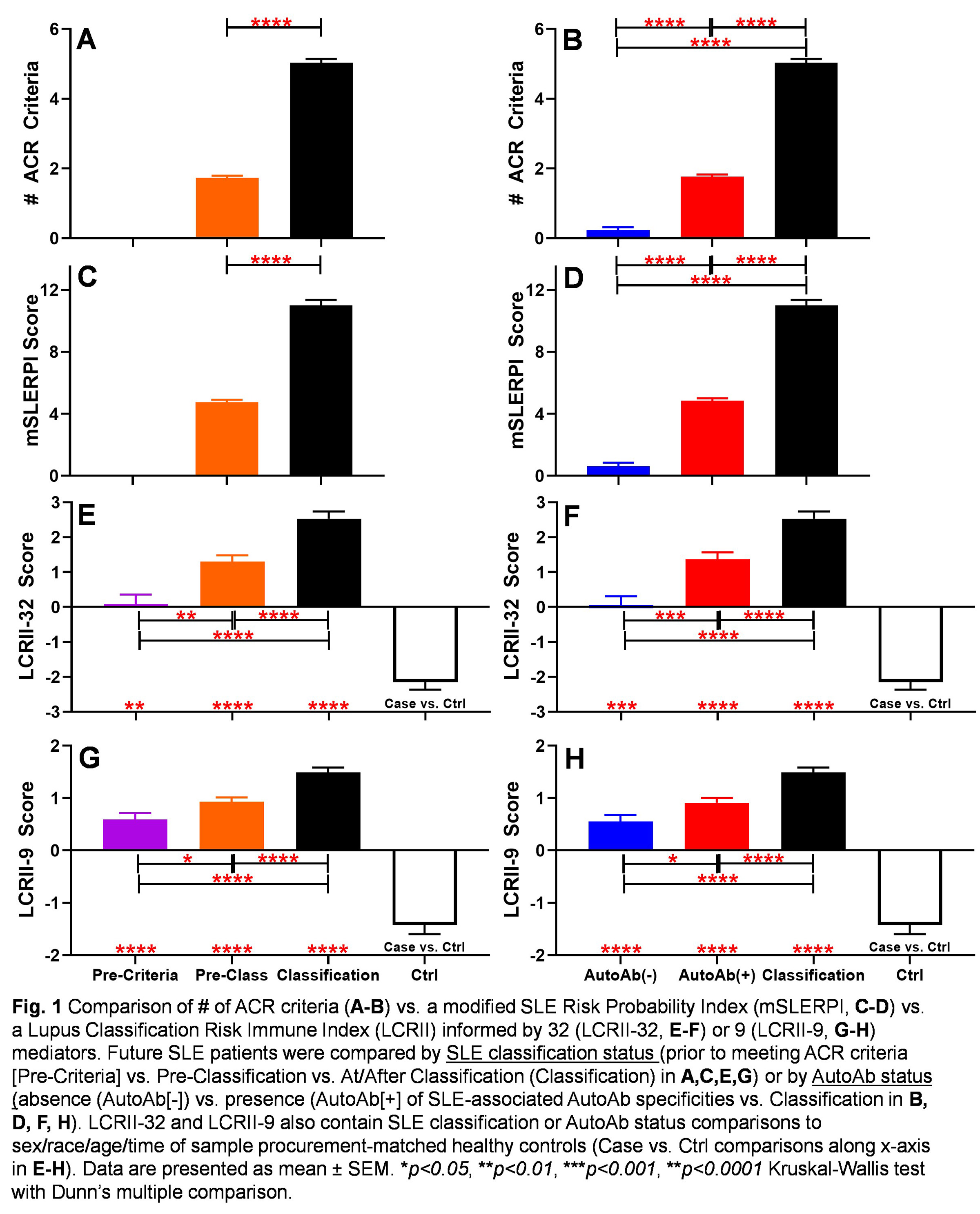
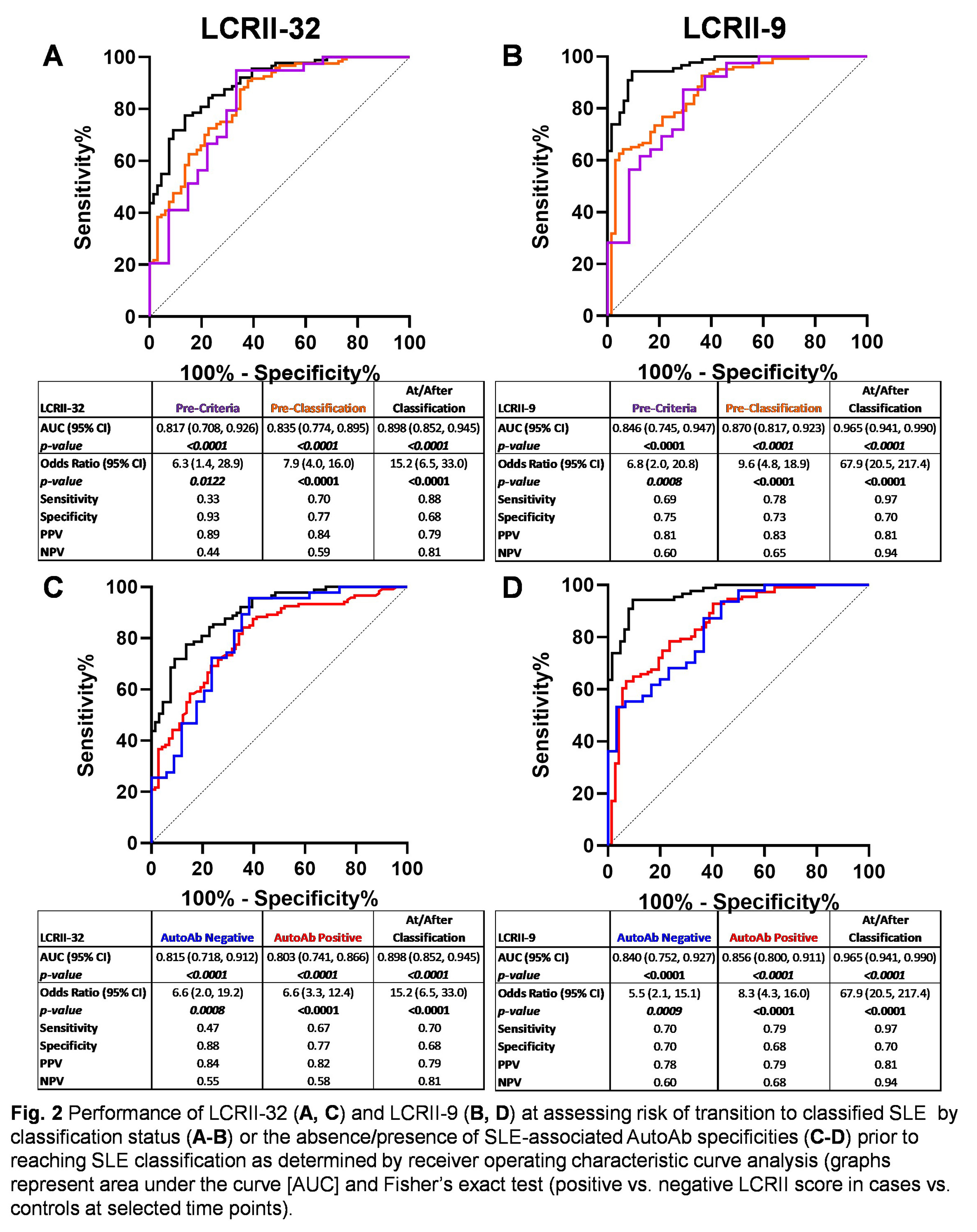
Methods: Sera from 84 SLE cases with serial specimens spanning from time points prior to 1997 ACR classification criteria through SLE classification (≥ 4 criteria; average timespan= 6.0 years) and matched healthy individuals (Ctrl) were obtained from the Department of Defense Serum Repository. Demographic, therapeutic, and ACR classification criteria were extracted from medical records. A modified version of the recent SLE Risk Probability Index (SLERPI; C. Adamichou et al. Ann. Rheum. Dis. 2021) was adapted to the 1997 ACR classification criteria (excluding alopecia, complement, and interstitial lung disease components). Samples were tested for SLE-associated AutoAbs, including dsDNA, chromatin, Ro/SSA, La/SSB, Sm, SmRNP, and RNP, and 32 soluble immune mediators, including cytokines, chemokines, and soluble receptors. The LCRII is the sum of log-transformed, standardized immune mediators, weighted by the Spearman r correlation coefficient of mediator levels vs. the number of SLE-associated AutoAbs present and correlates with number ACR criteria present (Spearman r = 0.456, p< 0.0001) and mSLERPI (Spearman r = 0.463, p< 0.0001).
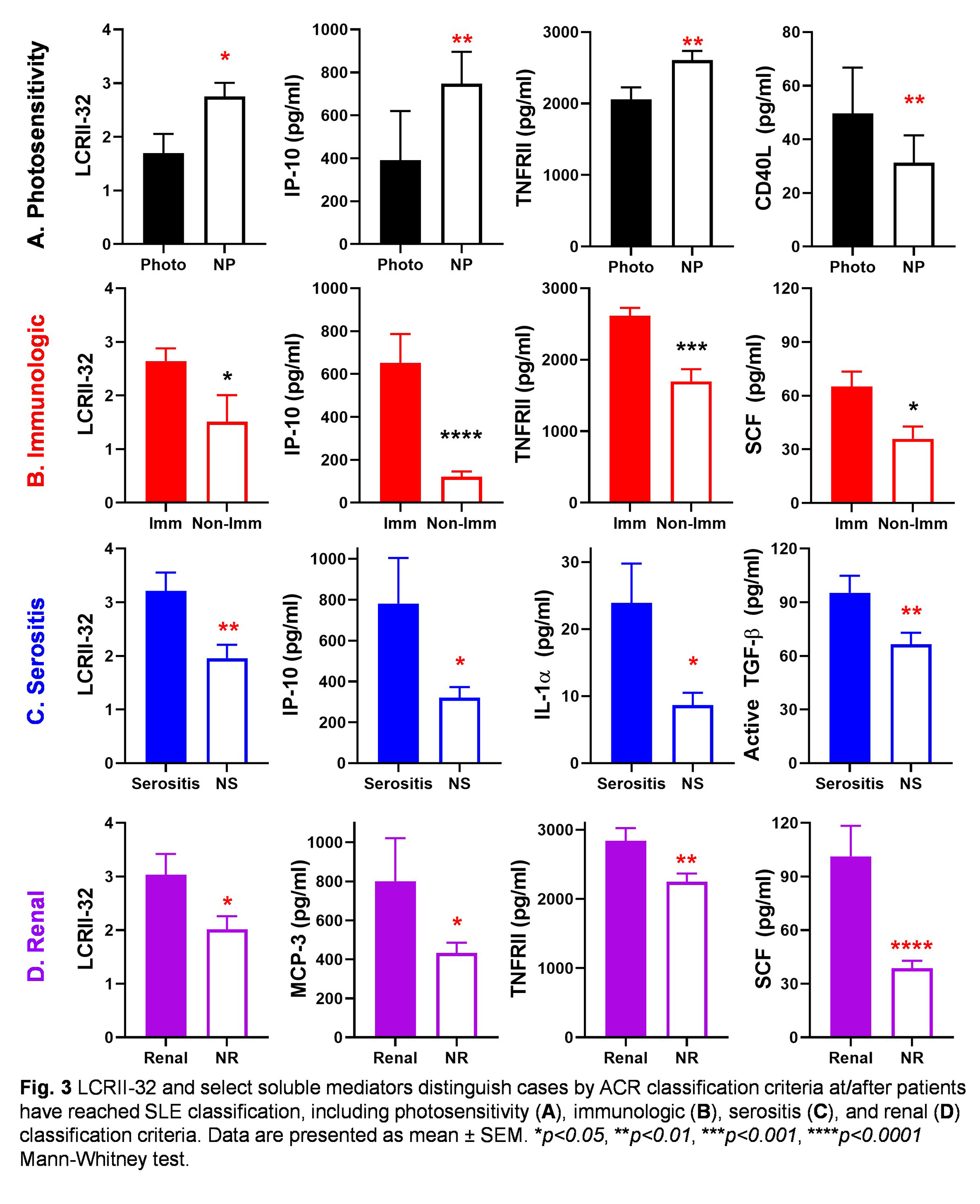
Results: Unlike ACR classification criteria and mSLERPI, future SLE patients could be identified in the absence of classification criteria (Pre-Criteria) using the LCRII informed by 32 immune mediators (LCRII-32, Fig 1). Of 32 mediators assessed, after correcting for multiple comparison (Bonferroni p≤0.0016), 9 were elevated during the Pre-Criteria phase compared to matched Ctrl, including adaptive mediators IL-12p70, IFN-γ, IL-4, IL-5, IL-17A, TGF-β, chemokines IP-10 and MCP-3, and plasminogen activator inhibitor-1 (PAI-1). Informing the LCRII with these 9 mediators (LCRII-9) did not reduce the ability of the LCRII to distinguish future SLE patients in the Pre-Criteria and AutoAb negative phases of SLE development (Fig 1). Overall, the LCRII-9 more clearly identified individuals by classification and AutoAb status (Fig 2). On average, future SLE patients met their first clinical criterion 6.4 months before reaching disease classification. In addition to the immunologic criterion, LCRII-32 and select informative mediator levels were altered in initial univariate analyses with select clinical features, including photosensitivity, serositis, and renal criteria (Fig 3). Neither hydroxychloriquine nor steroid use at/after SLE classification impacted the LCRII.
Conclusion: Clinically notable components of immunological profiles may help elucidate disease pathogenesis and help identify individuals at risk for developing SLE for clinical monitoring, early intervention, and enrollment in prevention trials.
To cite this abstract in AMA style:
Munroe M, Lu R, Gross T, Tsokos G, Keith M, Harley J, James J. Ability of Soluble Immune Mediators and SLE-associated Autoantibody Specificities to Forecast Transition to Classified SLE and Inform a Lupus Classification Risk Immune Index [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/ability-of-soluble-immune-mediators-and-sle-associated-autoantibody-specificities-to-forecast-transition-to-classified-sle-and-inform-a-lupus-classification-risk-immune-index/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ability-of-soluble-immune-mediators-and-sle-associated-autoantibody-specificities-to-forecast-transition-to-classified-sle-and-inform-a-lupus-classification-risk-immune-index/