Session Information
Date: Monday, November 18, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Previous studies have demonstrated that idiopathic inflammatory myopathy (IIM) is associated with an elevated cancer risk. However, there is limited evidence on the specific risk factors and effective risk-stratification for cancer in patients with IIM.
Methods: This study included 372 patients with IIM (including dermatomyositis, polymyositis, immune-mediated necrotizing myositis, overlap myositis, and anti-synthetase syndrome) from three independent cohorts in South Korea. Data on the history of previous malignancies, demographic/clinical features at the time of diagnosis, and response to initial immunosuppressive treatment were collected. Myositis specific and associated antibodies were assessed in all patients using the EUROIMMUN line immunoblot assay. The primary outcome was occurrence of myositis-associated cancer, defined as that occurred within 3 years before and after the diagnosis of IIM. Binary logistic regression analysis was used to identify relevant clinical factors associated with the outcome. The final prediction model was determined using a backward selection method. A scoring system to classify patients according to their predicted risk was established based on β coefficient of the final model. Conditional inference trees were employed to determine optimal cutoff values of the score, enabling precise risk stratification.
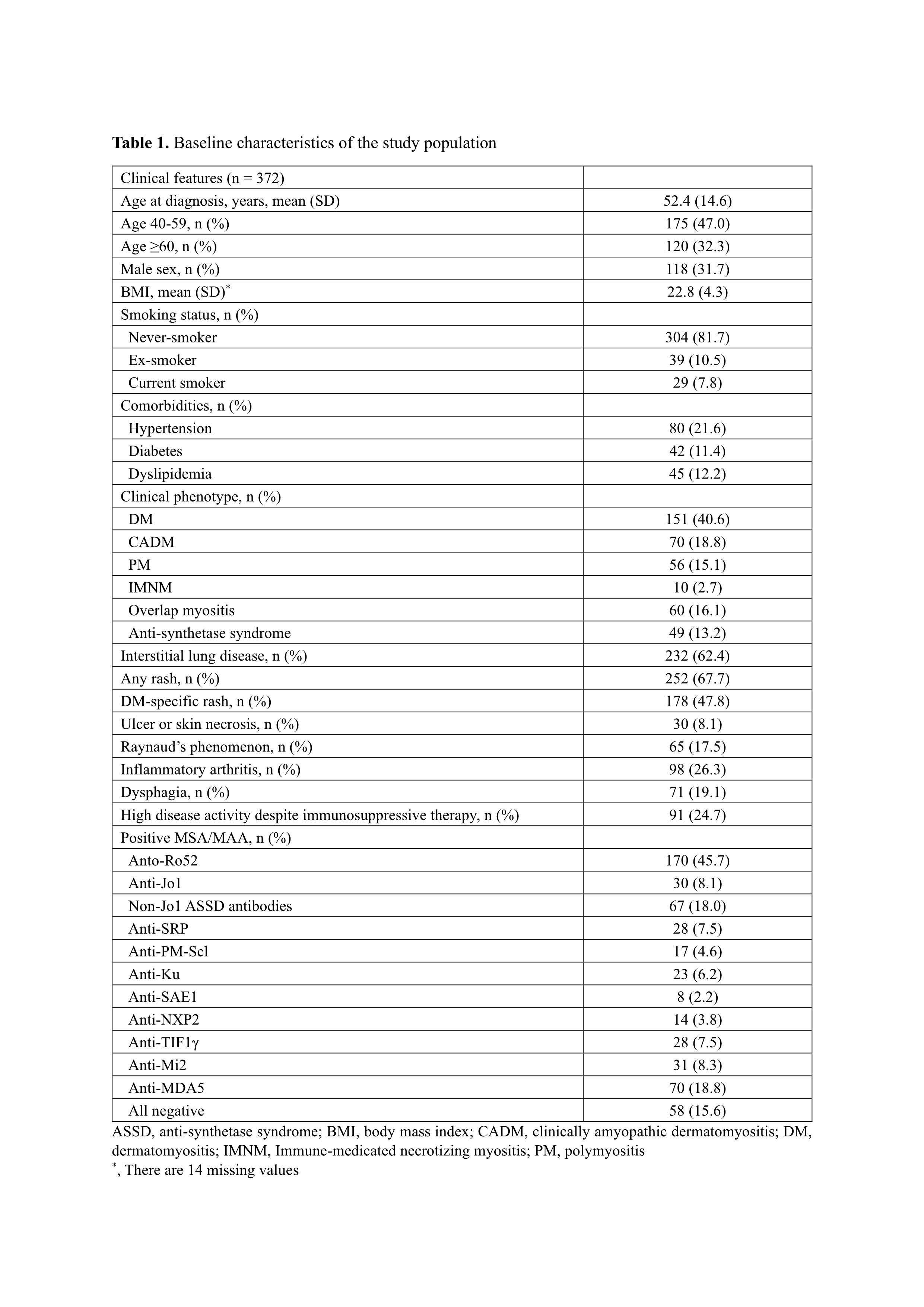
Results: Baseline characteristics of the patients were described in the Table 1. Mean (SD) follow-up duration from the time of IIM diagnosis was 5.7 (6.3) years. Fifty-eight cancer cases were captured, with 41 of them were myositis-associated. Most of myositis-associated cancers (n = 35, 85.4%) occurred within 1 year before and after the diagnosis of IIM.
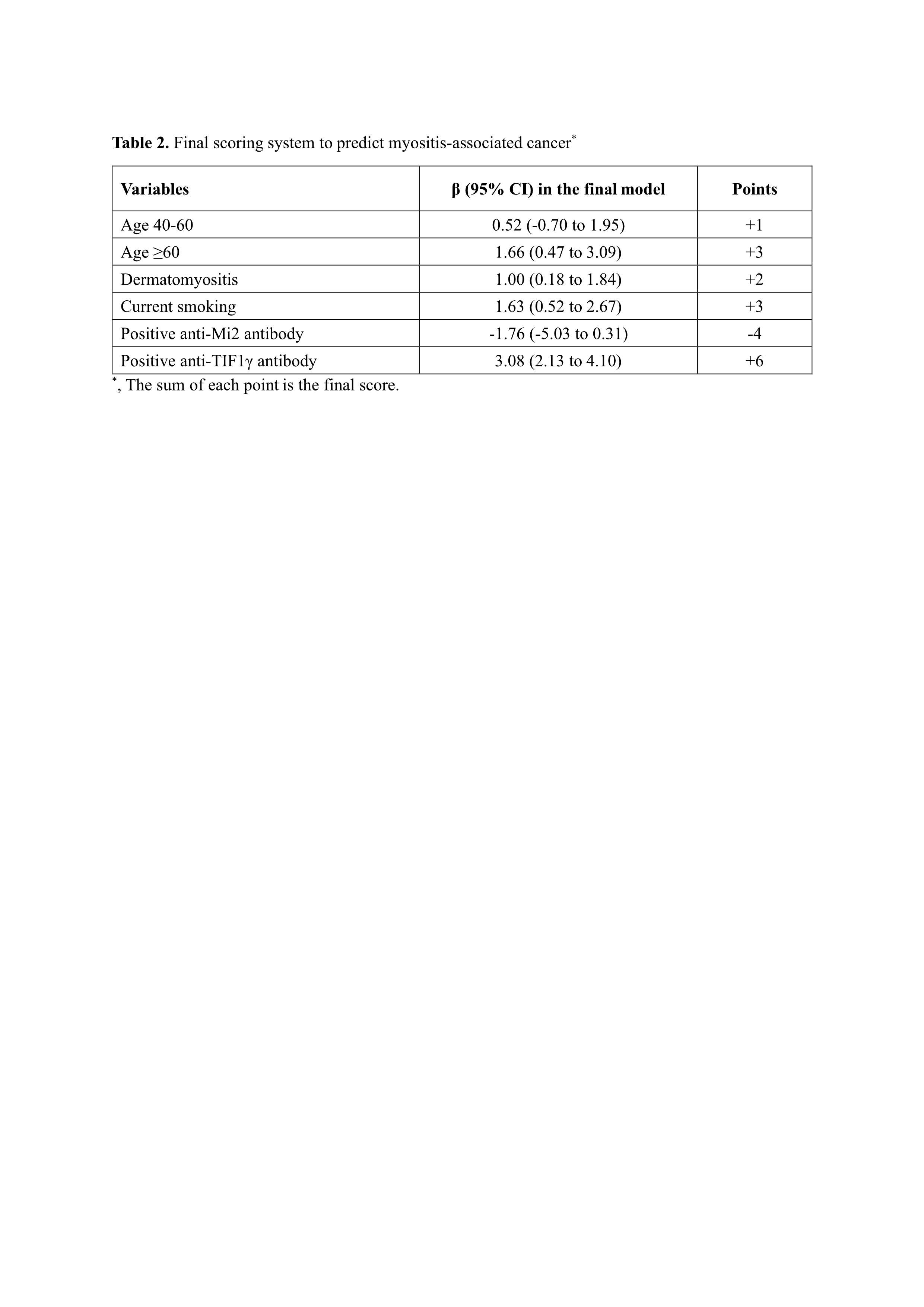
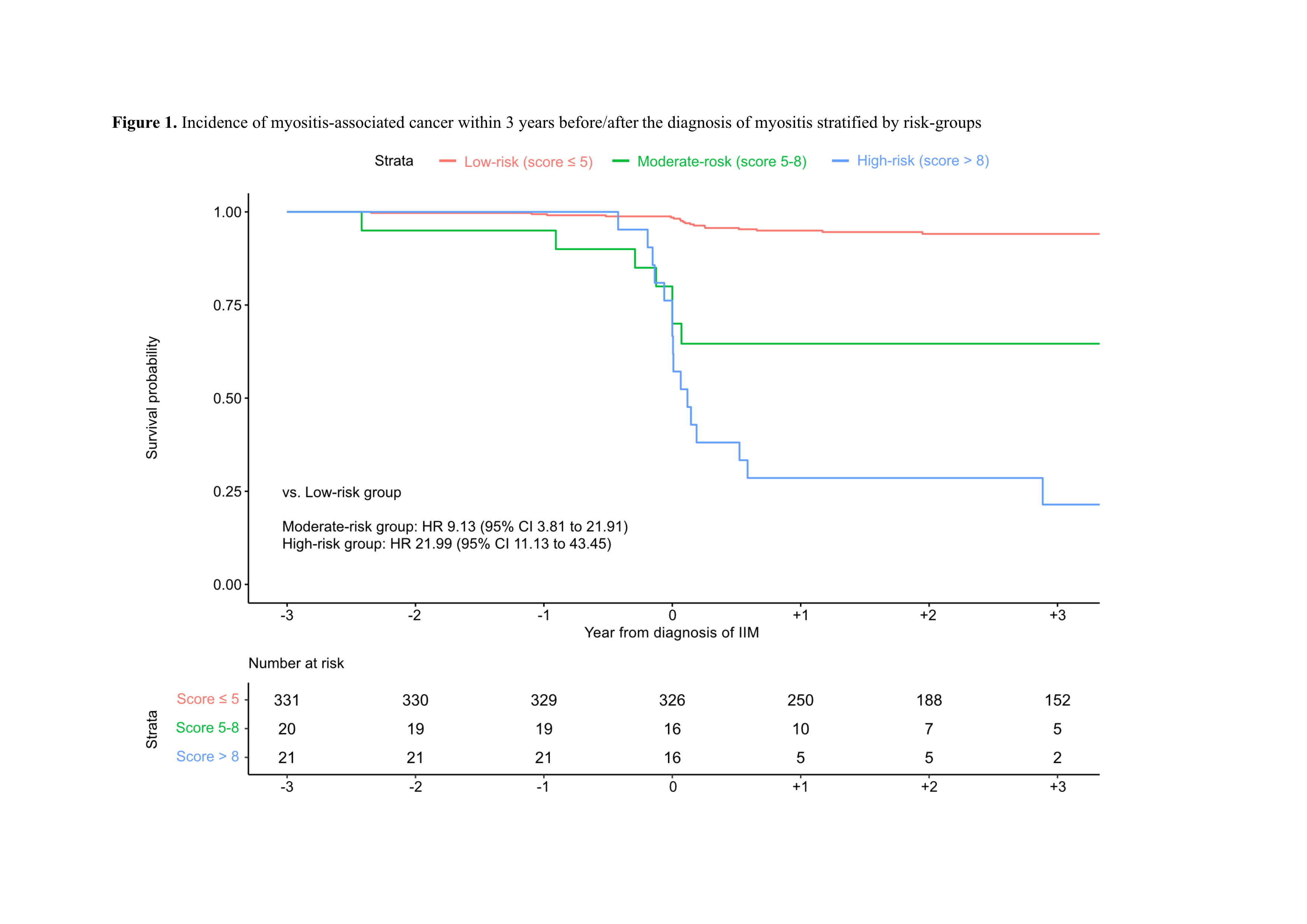
In the univariable analysis, old age (≥60 years), male sex, current smoking, dysphagia at the time of diagnosis, and dermatomyositis were associated with the primary outcome. Positive anti-TIF1γ markedly increased the risk of myositis-associated cancer (OR 25.12 [95% CI 10.63 to 62.80]) whereas positive anti-MDA5 and anti-Mi2 were associated with a lower incidence of cancer (OR 0.20 [0.03 to 0.67] and 0.25[0.01 to 1.22], respectively). Other clinical factors such as anti-NXP2, poor treatment response and cutaneous ulcer/necrosis were not significantly associated with the outcome. The final prediction model included age at diagnosis (< 40, 40-60, ≥60 years), current smoking, dermatomyositis, anti-TIF1γ and anti-Mi2 as variables (Table 2) and showed an excellent performance with an AUC of 0.839 (0.771 to 0.906). According to the scoring system, patients were classified into 3 groups based on the final score (low-risk group: score ≤5, moderate-risk group: score 5-8, high-risk group: score >8). Patients with moderate- and high-risk groups showed significantly higher incidence of myositis-associated cancer compared to those in the low-risk groups (adjusted HR 9.13 [3.81 to 21.91] and 21.99 [11.13 to 43.45], respectively) (Figure 1).
Conclusion: Our scoring system accurately quantified the risk of myositis-associated cancer in patients with IIM.
To cite this abstract in AMA style:
Kim Y, Kim J, Pyo J, Kim M, Park J, Lee E, lee Y, Lee e, park J. A Novel Scoring System to Predict a Cancer Development in Patients with Idiopathic Inflammatory Myopathy [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/a-novel-scoring-system-to-predict-a-cancer-development-in-patients-with-idiopathic-inflammatory-myopathy/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-novel-scoring-system-to-predict-a-cancer-development-in-patients-with-idiopathic-inflammatory-myopathy/