Session Information
Date: Sunday, November 12, 2023
Title: Abstracts: RA – Diagnosis, Manifestations, & Outcomes I: RA-ILD
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Based on the overlap in peripheral blood biomarkers associated with rheumatoid arthritis interstitial lung disease (RA-ILD) and idiopathic pulmonary fibrosis (IPF), a composite biomarker score based on IPF-molecular profiles was previously derived that correlated with RA-ILD disease stage (Kass et al. Arth Rheum, 2022; 74(suppl 9)). In this study, we aimed to externally validate the predictive value of a modified version of this biomarker score with prevalent and incident ILD in a large, multicenter RA cohort.
Methods: We performed cross-sectional and longitudinal analyses of participants in the Veterans Affairs Rheumatoid Arthritis registry, a prospective cohort of U.S. veterans with RA. RA-ILD diagnoses were validated by medical record review, with prevalent and incident ILD defined pre- and post-enrollment, respectively. Concentrations of 7 of 8 previously proposed IPF mediators (matrix metalloproteinase [MMP]-7, MMP-9, eotaxin, macrophage-derived chemokine [MDC], monocyte chemoattractant protein-1 [MCP-1], Fms-like tyrosine kinase 3 ligand [Flt3L] and interleukin-8 [IL-8]; MMP-2 unavailable and not included) were measured from serum/plasma at enrollment (MesoScale Discovery platform). Log-transformed and standardized values (per cohort mean and standard deviation for each analyte) were summed to compute a composite biomarker score. Associations of the biomarker score (continuous and quartile) with prevalent and incident RA-ILD were assessed in multivariable regression models (logistic and Cox), adjusted for age, sex, race, smoking status, anti-CCP positivity, and RA disease activity. Discrimination of prevalent RA-ILD was evaluated with receiver operating characteristic (ROC) curves, initially using the aforementioned clinical predictors alone and subsequently with the addition of the biomarker score.
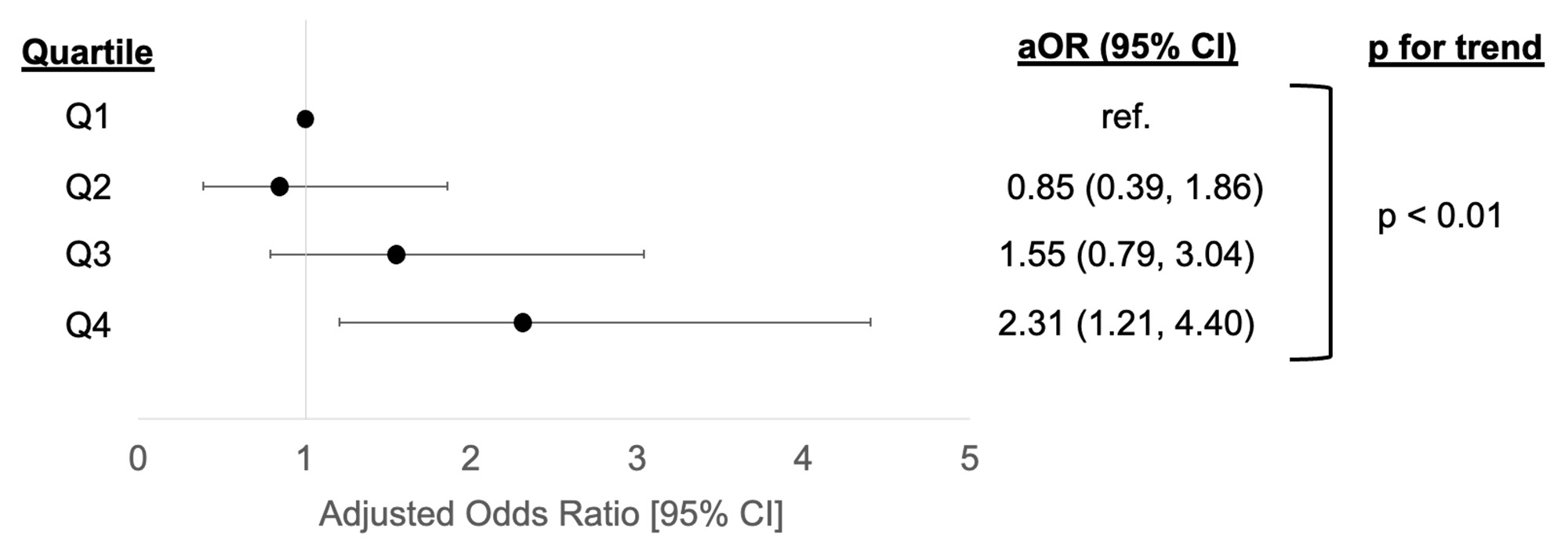
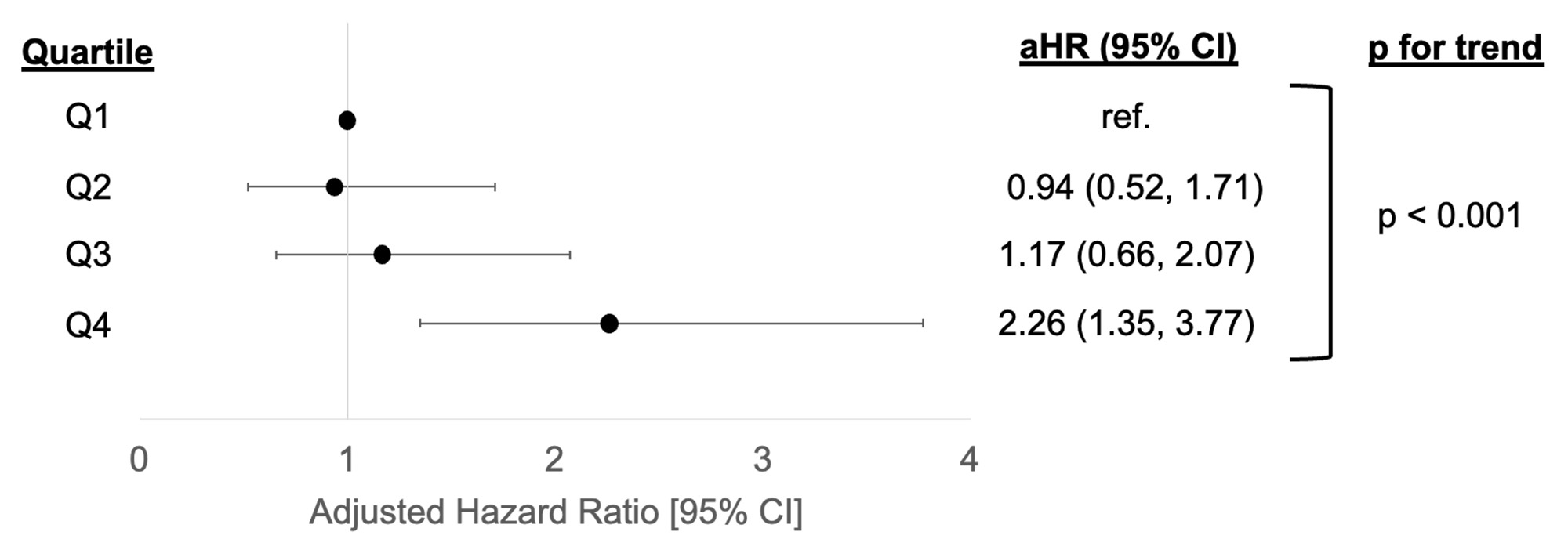
Results: Among 2,092 participants (89% male, mean age 64 years), prevalent RA-ILD was identified in 86 and incident RA-ILD developed in 116 participants during a mean follow-up of 7.7 years. Mean composite biomarker scores were significantly lower in participants without RA-ILD than in those with prevalent ILD or incident RA-ILD (-0.35 vs. 0.89 and 0.54, respectively, both p < 0.02). Higher biomarker scores were significantly associated with prevalent (aOR 1.08 [1.01, 1.15]) and incident (aHR 1.06 [1.01, 1.12] per 1 point increase) RA-ILD. Participants with biomarker scores in the highest quartile had over 2-fold higher odds of prevalent RA-ILD (Figure 1) and risk of incident RA-ILD (Figure 2). The addition of the biomarker score to clinical predictors did not significantly improve prevalent RA-ILD discrimination (AUC 0.653 [0.595, 0.711] clinical vs. 0.669 [0.613, 0.725] clinical and biomarker score, p = 0.30).
Conclusion: A modified composite biomarker score based on IPF molecular profiles was associated with prevalent and incident ILD in a large, multicenter RA cohort. While externally validating prior findings by Kass et al. and implicating IPF mediators in RA-ILD pathogenesis, the IPF-derived composite biomarker score had modest discriminative performance. Further work is needed to evaluate the clinical utility of this, and other, RA-ILD risk scores.
Models adjusted for age, sex, race, smoking status, anti-citrullinated peptide antibody status, and rheumatoid arthritis disease activity (28-joint disease activity score [DAS28]).
Abbreviations: ILD = interstitial lung disease, RA = rheumatoid arthritis, aOR = adjusted odds ratio, ref. = referent
Models adjusted for age, sex, race, smoking status, anti-citrullinated peptide antibody status, and rheumatoid arthritis disease activity (28-joint disease activity score [DAS28]).
Abbreviations: ILD = interstitial lung disease, RA = rheumatoid arthritis, aHR = adjusted hazard ratio, ref. = referent
To cite this abstract in AMA style:
Luedders B, Ascherman D, Kass D, Baker J, Duryee M, Yang Y, Roul P, Wysham K, Monach P, Reimold A, Kerr G, Kunkel G, Cannon G, Poole J, Thiele G, Mikuls T, England B. A Modified Idiopathic Pulmonary Fibrosis-Derived Composite Biomarker Score Is Associated with Interstitial Lung Disease Among U.S. Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-modified-idiopathic-pulmonary-fibrosis-derived-composite-biomarker-score-is-associated-with-interstitial-lung-disease-among-u-s-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-modified-idiopathic-pulmonary-fibrosis-derived-composite-biomarker-score-is-associated-with-interstitial-lung-disease-among-u-s-veterans-with-rheumatoid-arthritis/