Session Information
Date: Monday, November 9, 2020
Session Type: Abstract Session
Session Time: 4:00PM-4:50PM
Background/Purpose: Dietary restriction of short-chain fermentable oligosaccharides, disaccharides, monosaccharides and polyols (low FODMAP) has been found to reduce GI symptoms in patients with IBS and is often recommended to patients with SSc. However, no studies have evaluated whether a low FODMAP diet leads to a meaningful improvement in GI symptoms in patients with SSc. The purpose of this study was to (1) compare GI symptoms in SSc patients adhering to a low versus high FODMAP diet, and (2) determine whether GI microbial composition is altered in SSc patients adhering to a low FODMAP diet.
Methods: Adult patients satisfying the 2013 ACR/EULAR Classification Criteria for SSc provided stool samples for 16S rRNA sequencing. Participants completed the Diet History Questionnaire (DHQ) II, a valid, 153-item food frequency questionnaire that assesses dietary recall in the past month. Forty DHQ II items were characterized as high FODMAP items using the Monash University FODMAP food database. Patients were dichotomized into low versus high FODMAP groups, and GI symptoms, as measured by the UCLA GIT 2.0, were compared between the two groups. Microbial community differences between the low and high FODMAP groups were assessed using 3 metrics of alpha diversity (richness, evenness, phylogenetic diversity), as well as beta diversity. Multivariate negative binomial models were used to identify differentially abundant bacterial genera in the high versus low FODMAP groups.
Results: Patients in the low (N=19) and high (N=16) FODMAP groups were similar in terms of age, %female, BMI, disease duration, %diffuse disease, smoking history and %small intestine bacterial overgrowth [SIBO] (Table 1). There were no significant differences in GIT 2.0 scores between the low and high FODMAP groups, although the scores for some of the domains (e.g., Reflux, Distension, Diarrhea) were numerically higher in the high FODMAP group; whereas scores for the constipation domain were similar for both groups. There were no significant differences in alpha diversity between the two groups on both univariate and multivariate analysis controlling for age, sex, SSc subtype, smoking, SIBO and disease duration. There was no significant difference in beta diversity between the two groups on univariate and multivariate analysis (Figure 1). Compared with the low FODMAP group, the high FODMAP group had increased abundance of Enterococcus, a genus considered in a number of studies to be pathobiont (Figure 2); however, in the multivariate analysis, there was no significant genus level differences between the two groups with the exception of Parvimonas enrichment in the low FODMAP group.
Conclusion: Evidenced-based dietary recommendations for SSc are lacking. This is the first study to examine the relationship between diet, GI symptoms, and GI microbial composition in patients with SSc. Although this was a small study, the results demonstrate that consuming a low FODMAP diet is not associated with significant alterations GI microbial composition, nor significant improvements in SSc-GI symptoms. Larger, prospective SSc-GI studies are needed to help guide the clinical management of this troubling and understudied dimension of SSc.
 Table 1. Demographics, clinical characteristics and GIT 2.0 scores of SSc patients.
Table 1. Demographics, clinical characteristics and GIT 2.0 scores of SSc patients.
 Figure 1. Beta diversity of the High (Red) and Low (blue) FODMAP group patients as demonstrated by principal coordinate analysis plots of the robust Aitchison distance. Each dot represents a patient sample. The P-value (0.264) was calculated by analysis of variance using distance matrices.
Figure 1. Beta diversity of the High (Red) and Low (blue) FODMAP group patients as demonstrated by principal coordinate analysis plots of the robust Aitchison distance. Each dot represents a patient sample. The P-value (0.264) was calculated by analysis of variance using distance matrices.
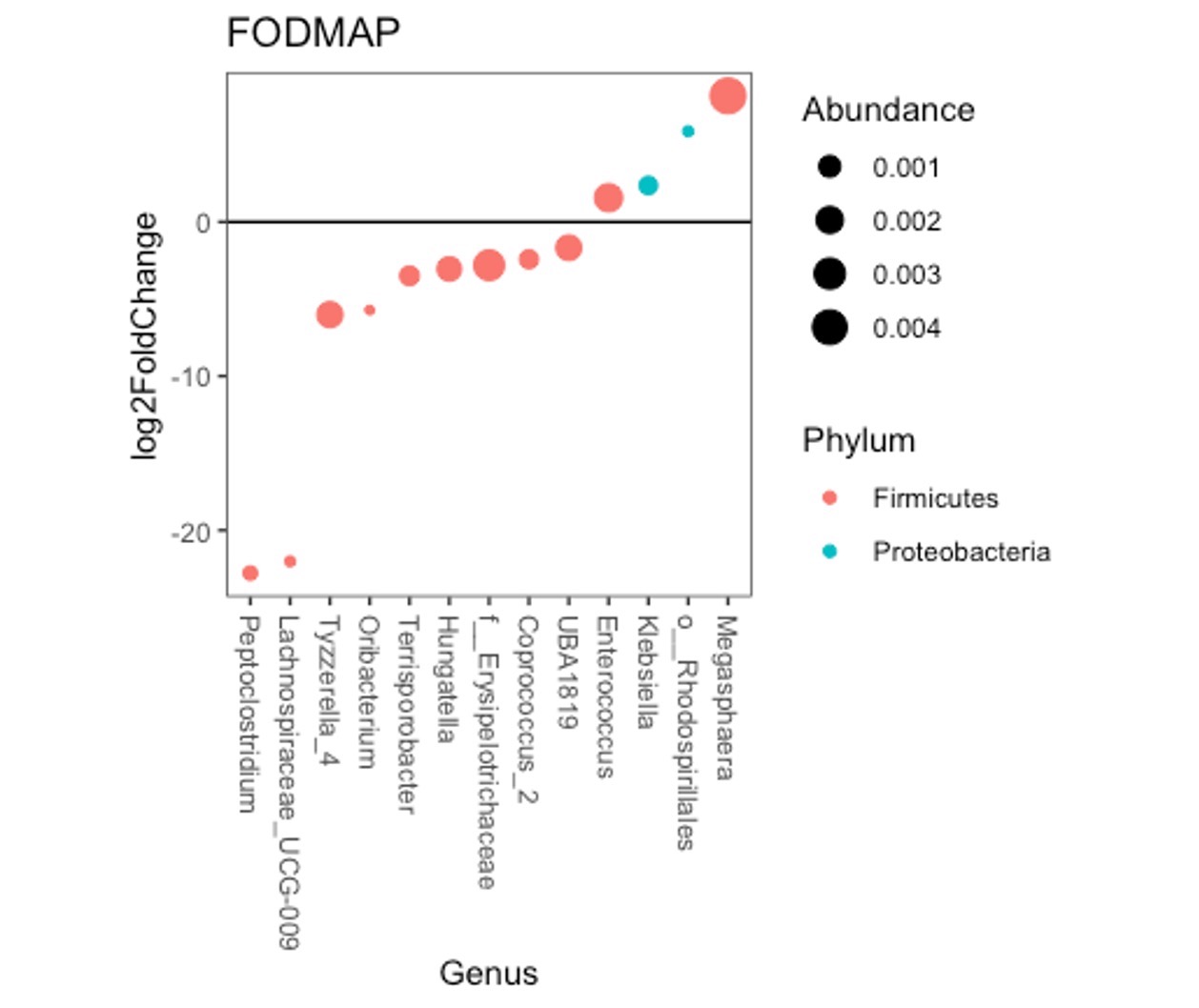 Figure 2. Genus level taxa with significant (q < 0.1) differential abundance between low versus high FODMAP groups. Circles with a positive fold change represent genera with increased abundance in the high FODMAP group, and circles with a negative fold change represent genera with increased abundance in the low FODMAP group. The color of the circle signifies the phylum level of the genera with differential abundance. The size of the circle indicates the relative abundance of the specific genus.
Figure 2. Genus level taxa with significant (q < 0.1) differential abundance between low versus high FODMAP groups. Circles with a positive fold change represent genera with increased abundance in the high FODMAP group, and circles with a negative fold change represent genera with increased abundance in the low FODMAP group. The color of the circle signifies the phylum level of the genera with differential abundance. The size of the circle indicates the relative abundance of the specific genus.
To cite this abstract in AMA style:
Howlett N, Lee S, Lagishetty V, McMahan Z, Wu M, Jacobs J, Volkmann E. A Low FODMAP Diet Is Not Associated with Decreased GI Symptoms or Changes in GI Microbial Composition in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/a-low-fodmap-diet-is-not-associated-with-decreased-gi-symptoms-or-changes-in-gi-microbial-composition-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-low-fodmap-diet-is-not-associated-with-decreased-gi-symptoms-or-changes-in-gi-microbial-composition-in-patients-with-systemic-sclerosis/
