Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: U2RNP is a spliceosome-associated autoantibody that has in prior case reports presented with scleroderma with myositis (SSc/PM)and SLE overlap. Autoantibodies are growing in prognostic importance in rheumatology and our center has performed immunoprecipitation for decades. There are few existing publications on U2RNP-associated disease features. This study aims to characterize disease phenotypes of U2RNP-positive patients.
We hypothesized based on limited available literature that patients positive for the anti-U2RNP autoantibody would display SSc features along with SLE or myositis characteristics compared to controls such as oral ulcers, thrombotic events, or cutaneous features.
Methods: This case-control study used our longstanding, prospectively followed SSc dataset. U2RNP patients initially seen in clinic between 1982 and 2015 were captured. Controls were the next two individuals seen without U2RNP (U2RNP-) Two-sided t-tests for continuous and Chi-squared tests for categorical variables were performed at a 95% confidence level.
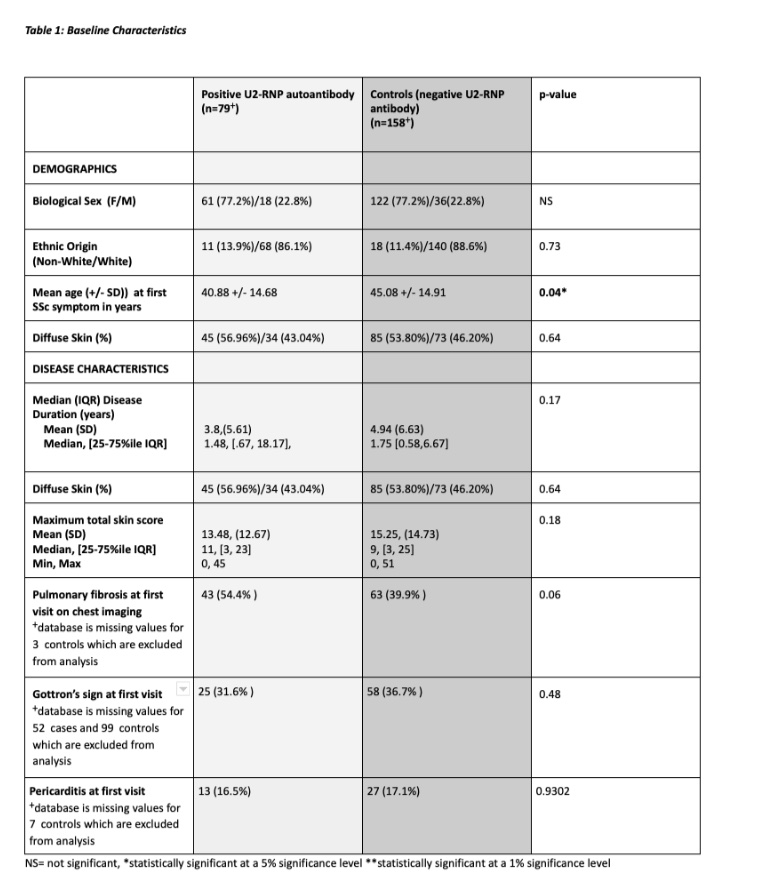
Results: 79 U2RNP+ and 158 U2RNP- patients were identified. There was no significant difference in proportion of non-white patients between groups. Mean age of symptom onset was earlier for U2RNP+ patients (mean 40.9, SD 14.7) than controls (mean 45, SD 14.9) with a p-value of 0.05 (Table 1).
Amongst U2RNP+ patients, 43% had diffuse skin thickening, similar to U2RNP- patients. We did not find a difference in rates of myositis between groups. Surprisingly, U2RNP- controls had a higher incidence of SLE-like features such as oral ulcers, thrombi, and pleurisy (Table 2). Only unspecified rashes differed significantly between groups (15.2% in U2RNP+ vs. 4.43% in U2RNP-, p = 0.0087). There was no difference in vascular comorbidities other than higher rate of MI in the U2RNP- group.
For SSc features, less U2RNP+ patients (26.92%) had telangiectasias than U2RNP- (70.9%; p < 0.0001). A larger percentage of individuals in the U2RNP+ group developed pulmonary fibrosis (57% vs. 44%, p = 0.12) in follow-up, and had pulmonary fibrosis at their first visit (54.4% vs. 39.9%, p = 0.06), though both findings related to fibrosis were not statistically significant. There was no difference in development and subtypes of pulmonary hypertension (Table 2).
Conclusion: This is the first large case-control study of patients with the anti-U2RNP antibody. Unlike U1RNP, U2RNP+ did not present with typical SLE or myositis features, aside from unspecified rash. Approximately 43% of U2RNP+ patients had diffuse skin thickening, but with less telangiectasias (27%). Though not statistically significant, there is a greater percentage of pulmonary fibrosis over the long-term and at initial visit in the U2RNP+ group. This finding may be further elucidated in further studies that match for age, biological sex, and other environmental factors that may influence fibrosis and perhaps guide screening recommendations for individuals who test positive for the autoantibody through serologies. The primary weakness is that this is a single-center study.
To cite this abstract in AMA style:
Dilip M, Laffoon M, Park Y, Lafyatis R, Medsger T, Steen V, Freno L, Domsic R. A Descriptive Study of Disease Characterisics of SSc Patients with the U2RNP Autoantibody [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-descriptive-study-of-disease-characterisics-of-ssc-patients-with-the-u2rnp-autoantibody/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-descriptive-study-of-disease-characterisics-of-ssc-patients-with-the-u2rnp-autoantibody/