Session Information
Date: Wednesday, October 29, 2025
Title: Abstracts: Rheumatoid Arthritis – Treatment II: Phenotyping and Personalization (2639–2644)
Session Type: Abstract Session
Session Time: 10:15AM-10:30AM
Background/Purpose: Patients with rheumatoid arthritis (RA) are at increased risk of major adverse cardiovascular events (MACE) and venous thromboembolism (VTE). Inflammation is a driver of vascular risk, but specific RA therapeutic classes may differentially influence this risk, especially among older patients with additional risk factors. We aimed to evaluate the association between RA medications and advanced therapy (AT) classes and the incidence of MACE and VTE.
Methods: RA patients were identified from the Ontario Rheumatoid Arthritis Database, a population-based registry derived using a validated algorithm and maintained at ICES. We included patients aged >67 years diagnosed between January 1, 2008, and December 30, 2013, and followed them through to December 30, 2023, with a minimum of 6 months follow-up. The primary outcome was healthcare utilization related to MACE (composite of myocardial infarction, stroke, congestive heart failure, and coronary artery bypass grafting) and/or VTE (deep vein thrombosis or pulmonary embolism), requiring hospital admission, emergency department (ED) visits, or physician encounters. RA therapeutic class was obtained from prescription data (Ontario Drug Benefit) and treated as a time-varying exposures into 4 mutually exclusive groups: (1) No csDMARDs or AT, (2) oral glucocorticoid (GC), (3) csDMARDs only (reference), or (4) b/tsSMARD (AT). The cohort was stratified by CVD risk, with high-risk individuals defined by the presence of established CVD, diabetes mellitus, or hypertension at RA diagnosis. The association between therapeutic class and recurrent healthcare encounters was assessed using the Andersen-Gill, an extension of the Cox model, adjusted for baseline covariates including concomitant csDMARD.
Results: A total of 10,020 RA patients were included and 80% had high CVD risk (n= 8,016). Over a median follow-up of 10.9 (IQR: 5.9-12.7) years, 16,468 MACE and 2,326 VTE events occurred in the high-risk group, compared to 2,965 MACE and 495 VTE events in the low CVD risk cohort. Compared to csDMARDs, there was a significant positive association between no csDMARD/AT (adjusted hazard ratio [aHR]: 13.3; 95% CI: 11.9, 14.8), oral GC (HR: 1.54; 95% CI: 1.26, 1.88), and higher hazard of MACE in the high-risk CVD cohort, while AT was associated with a lower hazard (adj HR: 0.63; 95% CI: 0.41, 0.99) (Table). Similar results were observed for no csDMARD/AT and oral GC in the low-risk CVD cohort. No csDMARD/AT and oral GC prescription were significantly associated with higher hospitalization/ED or physician visits for VTE compared to csDMARDs in both low and high CVD risk cohorts (Table). VTE events were numerically higher for AT users in the high CVD risk cohort, but this was not statistically significant.
Conclusion: In this study, therapeutic choice significantly influenced MACE and VTE outcomes. Compared to csDMARDs, advanced therapies were associated with a lower hazard, while GC and lack of RA treatment were associated with a higher hazard. These findings highlight the importance of integrating cardiovascular and thrombotic risk assessment into RA treatment decisions to optimize both disease and safety outcomes.
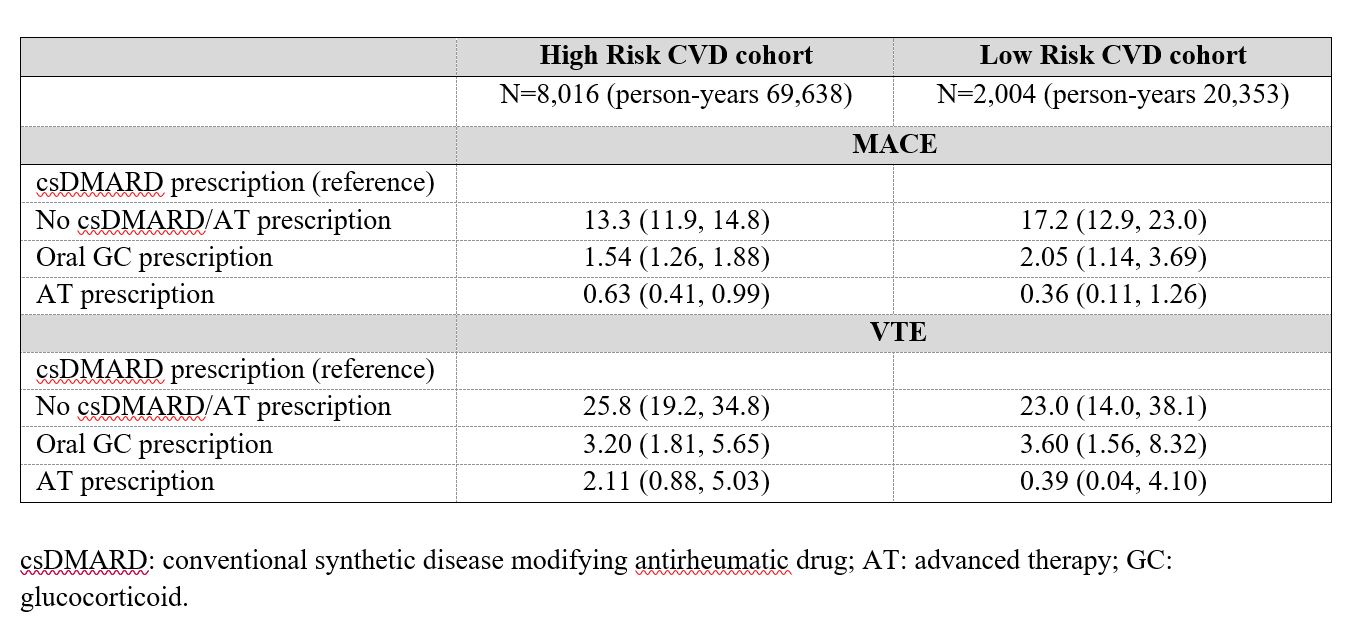 Table. Adjusted hazard ratios (HR) and 95% confidence intervals for healthcare utilization due to major adverse cardiovascular events (MACE) or venous thromboembolism (VTE) by RA therapeutic class and baseline cardiovascular (CVD) risk.
Table. Adjusted hazard ratios (HR) and 95% confidence intervals for healthcare utilization due to major adverse cardiovascular events (MACE) or venous thromboembolism (VTE) by RA therapeutic class and baseline cardiovascular (CVD) risk.
To cite this abstract in AMA style:
Movahedi M, Cesta A, Aydin S, Akhavan P, Kendzerska T, Bombardier C, Kuriya B. Impact of Rheumatoid Arthritis Therapeutic Classes on Risk of Major Adverse Cardiovascular Events and Venous Thromboembolism: A Population-Based Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-rheumatoid-arthritis-therapeutic-classes-on-risk-of-major-adverse-cardiovascular-events-and-venous-thromboembolism-a-population-based-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-rheumatoid-arthritis-therapeutic-classes-on-risk-of-major-adverse-cardiovascular-events-and-venous-thromboembolism-a-population-based-cohort-study/
