Session Information
Session Type: Abstract Session
Session Time: 3:45PM-4:00PM
Background/Purpose: People with axial spondyloarthritis (axSpA), typically present with persistent back pain and experience up to a 10-year diagnostic delay that may lead to irreversible spinal damage. Earlier diagnosis and treatment may prevent this damage. As such, there is a high clinical unmet need in primary care, to differentiate patients with axSpA who require a referral to a rheumatologist from those with mechanical backpain (MBP). According to the Spondyloarthritis Research and Treatment Network (SPARTAN), identifying 1 axSpA patient of 3 referred, could meaningfully reduce diagnostic delay. This study examines the discriminative performance of 14-3-3η AAbs in patients with axSpA, including those with radiographic (r-) and non-radiographic (nr-) disease, compared to people with MBP.
Methods: Patient serum (n=160) from the Bath Spondyloarthritis Biobank, a repository collected during routine clinical visits, were selected based on sample availability. Patients had a rheumatologist confirmed diagnosis and met classification criteria for r-axSpA (modified New York criteria, n=55), nr-axSpA (ASAS 2009 criteria, n=54) or MBP (n=51). 14-3-3η AAb levels were measured using the Health Canada and UKCA approved multiplex assay. Nominal regression was performed to model the relationship between predictor variables and diagnosis. The probability formula generated from this regression was used to calculate a linear score for three models alongside variables of age, sex, CRP and HLA-B27: 1) all patients with axSpA (n=109), 2) r-axSpA, and 3) nr-axSpA versus MBP as a control group. This score quantifies the likelihood of a diagnosis based on model predictors. The r-axSpA versus MBP regression was used to calculate 14-3-3η AAb scores in banked serum samples from healthy individuals (n=100) for comparison. Statistical significance was set at p < 0.05.
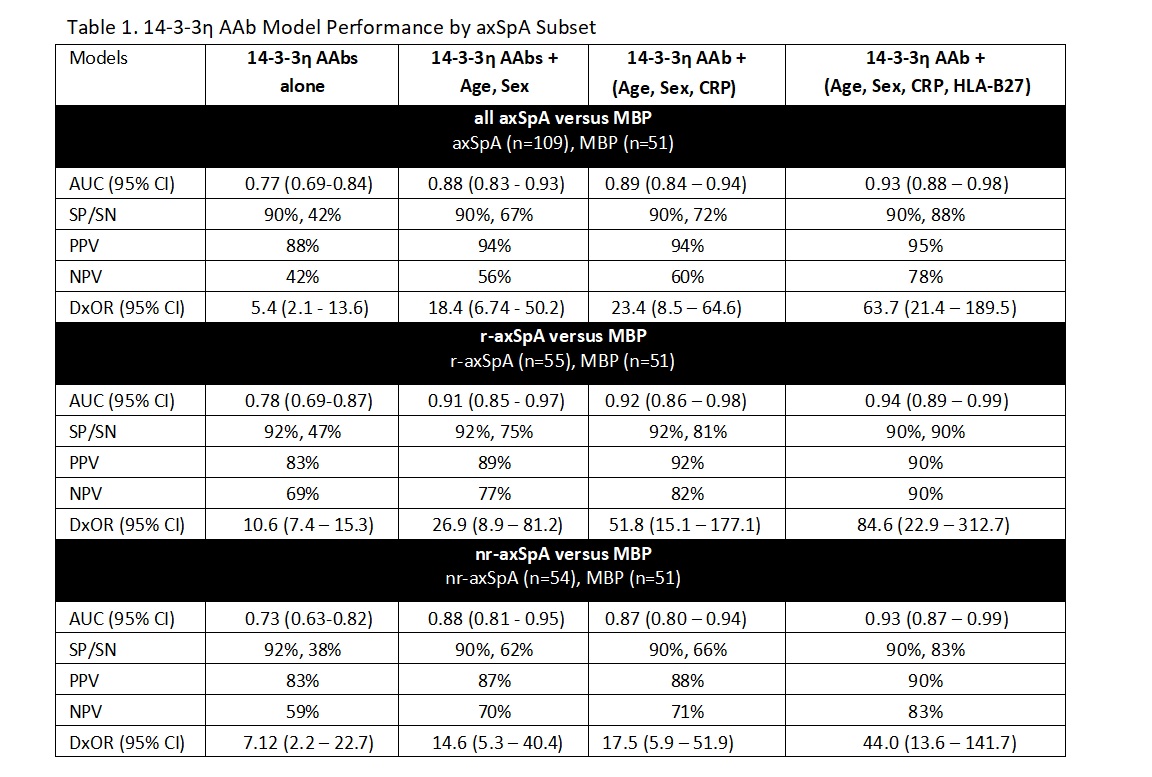
Results: Mean age (SD) was 55 (23) yrs for r-axSpA, 42 (14) yrs for nr-axSpA, and 30 (14) yrs for MBP. Gender distribution (% male) was respectively 67%, 41%, and 59%. Disease duration (SD) was 13 (27) yrs for r-axSpA, and 5 (5) yrs for nr-axSpA. HLA-B27+ status was: 69% for r-axSpA, 72% for nr-axSpA, and 18% for MBP. 14-3-3η AAb predictive model ROC AUCs for all axSpA versus MBP were 0.77, r-axSpA of 0.78 and nr-axSpA 0.73 (Table 1). Selecting the best sensitivity (SN) for ~90% specificity (SP) returned SP & SN for all axSpA of 90% & 42%, r-axSpA of 92% & 47% and nr-axSpA of 92% & 38%. Corresponding Positive Predictive Values (PPV) were 88%, 83% and 83%, exceeding the SPARTAN target 33.3% PPV. In the All axSpA model, adding age and sex variables to the 14-3-3η AAb score, improved the diagnostic odds ratio (DxOR) from 5.4 to 18.4 and increased to 23.4 with CRP added and to 63.7 with HLA-B27 added. Scores for healthy controls were similar to patients with MBP, p >0.99 (Figure 1).
Conclusion: The 14-3-3η AAb biomarker differentiates radiographic and non-radiographic-axSpA from MBP, achieves a high PPV and its discrimination improves when age, sex, CRP, and HLA-B27 are added. Alongside these easily accessible patient variables at primary care, 14-3-3η AAb may reduce diagnostic delay and complement HLA-B27.
To cite this abstract in AMA style:
Sengupta R, Marotta A, Maksymowych W, Cavill C, Bleakley S, Biln N. Autoantibodies to 14-3-3 eta: A Novel Diagnostic Biomarker for Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/autoantibodies-to-14-3-3-eta-a-novel-diagnostic-biomarker-for-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibodies-to-14-3-3-eta-a-novel-diagnostic-biomarker-for-axial-spondyloarthritis/

.jpg)