Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The complement system is known to play a central role in the pathogenesis of lupus nephritis (LN), one of the most severe manifestations of SLE. Emerging data suggest complement activation, particularly via membrane attack complex (MAC), mediates tubulointerstitial injury in LN. Studies have shown that tubulointerstitial damage leads to CKD progression in LN. Therefore, it is important to understand the mechanisms driving tubulointerstitial injury in LN to identify potential therapeutic targets. The objective of this study is to investigate C9 deposition, a part of the MAC, as a potential marker of tubulointerstitial injury and its association with chronic kidney disease (CKD) progression.
Methods: This retrospective cohort study included 30 LN patients who underwent kidney biopsies between February 2017 to November 2019 at an urban tertiary center. C9 deposition in proximal renal tubules was assessed via chromogenic immunohistochemistry on paraffin-embedded LN biopsy specimens stained with murine anti-human C9 antibody. C9 staining intensity was graded on a semi quantitative scale of 0 to 3 and categorized as present (1-3) vs absent (0). The percentage of staining in the tubules was also recorded. CKD progression was defined as >30% decline in estimated glomerular filtration rate (eGFR) within 5 years post biopsy, and those with stable or missing eGFR values were defined as non-progressors. Interstitial fibrosis/tubular atrophy (IFTA) was defined as >10% affected interstitium. Non-responders were defined as < 50% improvement in UPCR from baseline with no improvement in eGFR. CKD progression rates, treatment response, and IFTA were compared between C9 Positive (C9+) and C9 Negative (C9-).
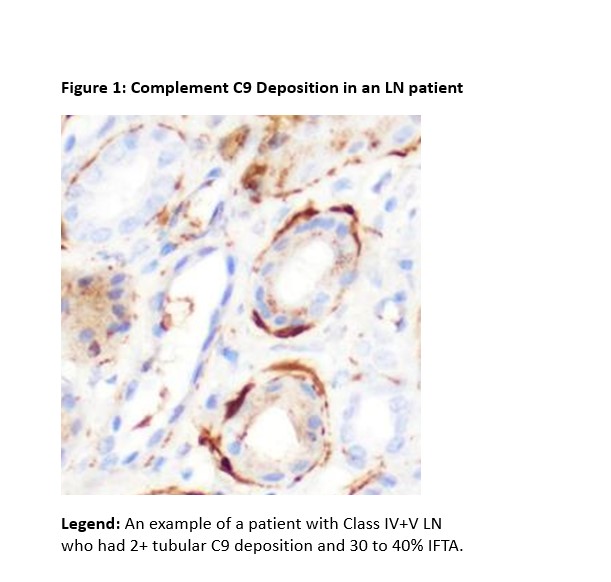
Results: Among 30 LN patients, mean (SD) age was 34 (10.3) years, 23 (77%) were women, and 17 (57%) had proliferative LN (Class III, IV, III+V, and IV+V). Eighteen (60%) had tubular C9 deposition and 10 (33%) progressed to CKD. An example of an LN patient with tubular C9 stain is shown in Figure 1. Tubular C9 deposition was associated with IFTA: 71% in the C9+ group vs. 25% in the C9- group (p=0.016). LN patients with IFTA had greater C9 stain intensity (mean (SD) 1.0(0.6) vs 0.39 (0.56)) and percentage of tubules with C9 stain (14.67% (13.95) vs 5.36% (8.43)) as compared to LN without IFTA. Compared with C9- group, C9+ group had a lower median (IQR) urine-to-protein ratio (1.5 (0.9, 3.1) vs. 3.5 (2.2, 4.8) g/g, p=0.04) [Table 1]. Kaplan-Meier curves showed longer times to CKD progression in C9- group, with separation of the curves occurring after 2 years [Figure 2]. There was no difference in eGFR, serum creatinine, and treatment response at 6 months between the two groups.
Conclusion: This study demonstrates an association between C9 deposition in kidney tubules of LN patients with tubulointerstitial fibrosis. Patients with higher tubular C9 intensity trended towards shorter renal survival although not statistically significant, likely due to limited sample size. These findings highlight tubular MAC deposition as a potential marker for IFTA and CKD progression, underscoring the complement pathway as a potential therapeutic target for tubulointerstitial disease in LN.
To cite this abstract in AMA style:
Lu A, Shao D, Jin Y, Chiriboga L, Wu M, Pullman J, Broder A, Wang S. Renal Tubular Complement C9 Deposition is Linked to Tubulointerstitial Fibrosis and Progression to Chronic Kidney Disease in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/renal-tubular-complement-c9-deposition-is-linked-to-tubulointerstitial-fibrosis-and-progression-to-chronic-kidney-disease-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-tubular-complement-c9-deposition-is-linked-to-tubulointerstitial-fibrosis-and-progression-to-chronic-kidney-disease-in-lupus-nephritis/

.gif)