Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Adolescents and young adults (AYAs) with rheumatic diseases require specialized care, particularly when transitioning from pediatric to adult healthcare. However, most residents and fellows receive little to no formal education in AYA care. One study found that over half of internal medicine trainees reported no instruction in AYA transition care, resulting in low confidence and potentially suboptimal patient outcomes. Targeted, high-quality transition education has been shown to improve trainee performance, but data on rheumatology fellowship training remain limited.
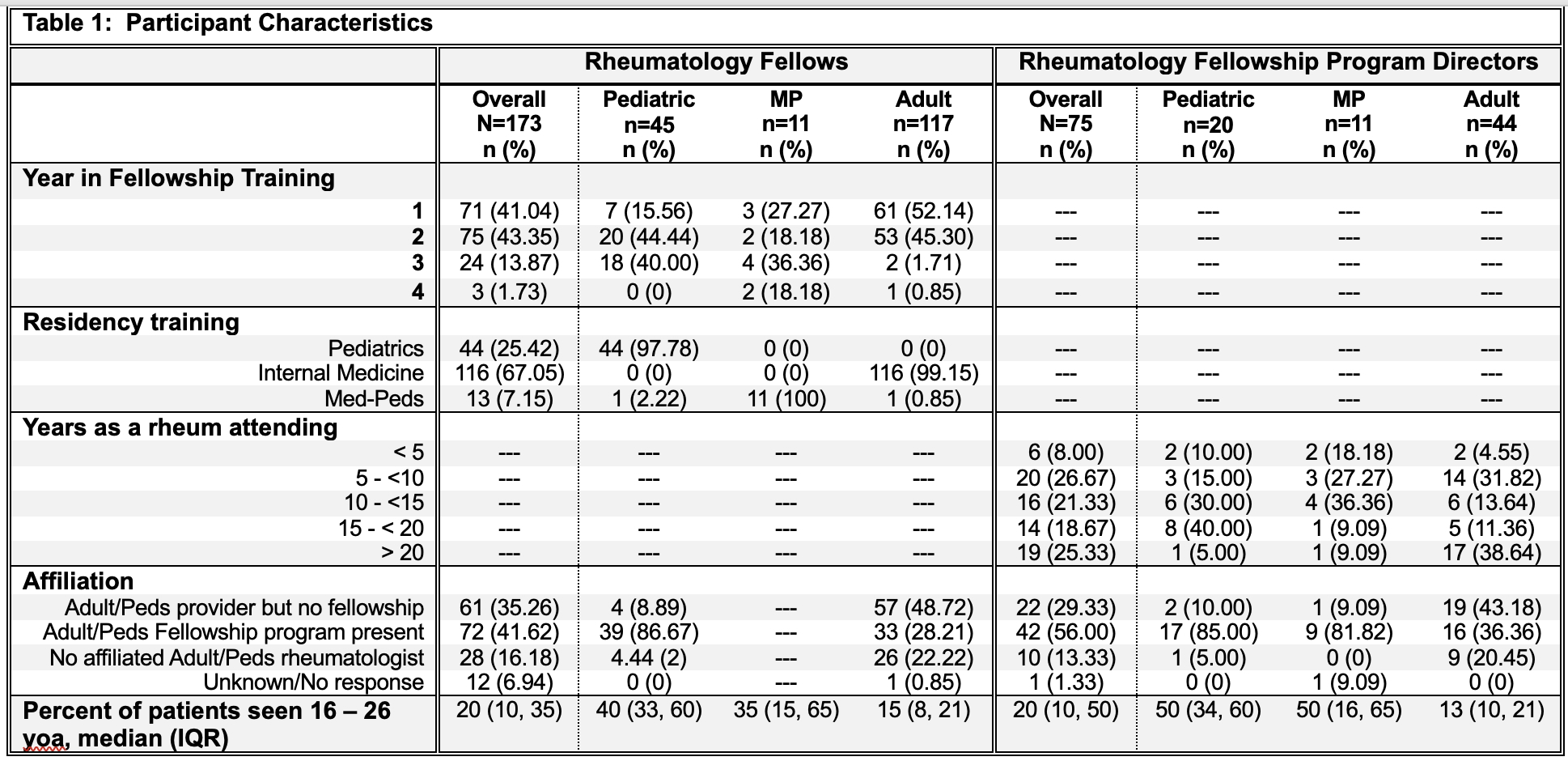
Methods: A national survey of pediatric, adult, and med-peds (MP) rheumatology fellows and program directors (PDs) was conducted from 2/2024–7/2024 to assess AYA training, priorities, exposure, beliefs, confidence, and practices. Survey items used Likert scales. Quality of AYA education and clinical tools was assessed using weighted scoring systems (high-quality education: exposure to ≥4 education techniques; high-quality transition tools: use of ≥3 transition tools). Fellows were considered prepared if ≥66% of skill items were endorsed as “prepared” or “completely prepared.” Frequent AYA best practice use was defined as performing ≥4/7 care tasks ≥60% of the time. Data was analyzed descriptively and with non-parametric approaches.
Results: Surveys were distributed to 167 programs (130 adult, 37 pediatric/MP). Of those, 75 PDs and 173 fellows responded (47% and 29% response rates, respectively). Among respondents, 22% of adult fellows and 20% of adult PDs lacked an affiliated pediatric rheumatologist. Adult PDs estimated only 13% of their patients were aged 16–26 years, compared to 50% for pediatric/MP PDs; fellows reported similar trends (Table 1). All respondents rated AYA topics (transition, reproductive health, bone health, cardiovascular disease risk, vaccination) as important for training. Only 38% of adult fellows felt prepared to optimally care for AYA patients vs. 64% of pediatric/MP fellows. Preparedness was highest among MPs (Table 2). Fellows caring for more AYA patients reported greater preparedness.Pediatric/MP fellows reported more diverse and higher quality AYA education than adult fellows (61% vs. 39%). Exposure to high-quality education was associated with more frequent AYA best practice use in pediatric/MP fellows, compared to those who received lower quality education (68% vs. 32%), but less so with self-reported preparedness.Pediatric/MP fellows reported more access to high-quality transition tools (Figure 1) than adult fellows (50% vs. 17%). Additionally, pediatric/MP fellows with access to these tools used clinical best practices more frequently than those without (55% vs. 45%).
Conclusion: Despite broad recognition of the importance of AYA care, rheumatology fellowship training in these skills remains insufficient, especially in adult programs. Direct exposure to AYA patients, access to high-quality education and clinical tools, and MP training were all associated with increased preparedness and best practice adherence. A standardized, structured framework for AYA-focused training is needed to prepare rheumatology trainees to best care for this vulnerable patient population.
To cite this abstract in AMA style:
Moyer A, Tandel M, Benjamin M, Lu R, Simard J, Sadun R. Bridging the Gap: A National Needs Assessment of Rheumatology Fellowship Training in Adolescent and Young Adult Care [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/bridging-the-gap-a-national-needs-assessment-of-rheumatology-fellowship-training-in-adolescent-and-young-adult-care/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bridging-the-gap-a-national-needs-assessment-of-rheumatology-fellowship-training-in-adolescent-and-young-adult-care/

.jpg)
.jpg)