Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile scleroderma (JS) is an autoimmune disease that can cause skin sclerosis leading to deformity, disability, and early mortality especially with delayed diagnosis. A general needs assessment performed by the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Scleroderma Workgroup identified gaps in provider medical knowledge as the main barrier to diagnosis and treatment of the child, from the caregiver perspective. The aim of this study is to characterize the knowledge gap, barriers to referral and preferred educational methods to inform the production of provider-facing educational materials. The researchers hypothesize that pediatric primary care providers harbor low awareness and disease misconceptions regarding JS.
Methods: A targeted needs assessment was built to survey providers in pediatrics, family medicine, and dermatology. After 8 rounds of expert review, pilot testing with 7 physicians, and approval by the Washington University Institutional Review Board, the consent and survey were distributed through email invitation to provider groups and on social media. Providers were recruited and consented via email to participate in 15-minute-long interviews to better understand providers’ knowledge and preferences for education on JS. Interviews were recorded, transcribed, and inductively analyzed by 3 team members to reduce bias.
Results: 88 of 1092 invited providers (8%) from all 5 geographic regions of the United States (Figure 1) responded to the survey, with 58 physicians out of training, 25 physicians-in-training, and 5 advanced practice providers. The responses came from 63 providers in pediatrics, 10 in family medicine, and 14 in dermatology. 24% of respondents didn’t know or thought that juvenile localized scleroderma (jLS) was not a serious disease (Figure 2). 38% didn’t know or thought jLS would burn out without needing treatment. 49% either didn’t know or thought some jLS patients do not need to see pediatric rheumatology. 5/12 participants that treat jLS incorrectly chose the most common subtype of jLS. 38% of providers felt that rheumatology wait list was a barrier to referral. 70% felt that additional education in scleroderma would be very or somewhat useful (Figure 3). 65% preferred an interactive online module for education and 70% preferred it be less than 15 minutes in duration. The qualitative analysis identified time and low prioritization on rare conditions as barriers to education on scleroderma, recommended education be focused on presenting features, and conference presentations as preferred delivery.
Conclusion: This study demonstrates knowledge gaps regarding JS among pediatric primary care providers. Opportunities for education include the presentation and seriousness of the disease in children, and differences from adult disease. Limitations of this study include limited responses and response bias. Next steps include making educational resources such as a brief interactive module to address the gap and reduce barriers to referral. This has the potential to increase early diagnosis, which would improve outcomes of children with JS.
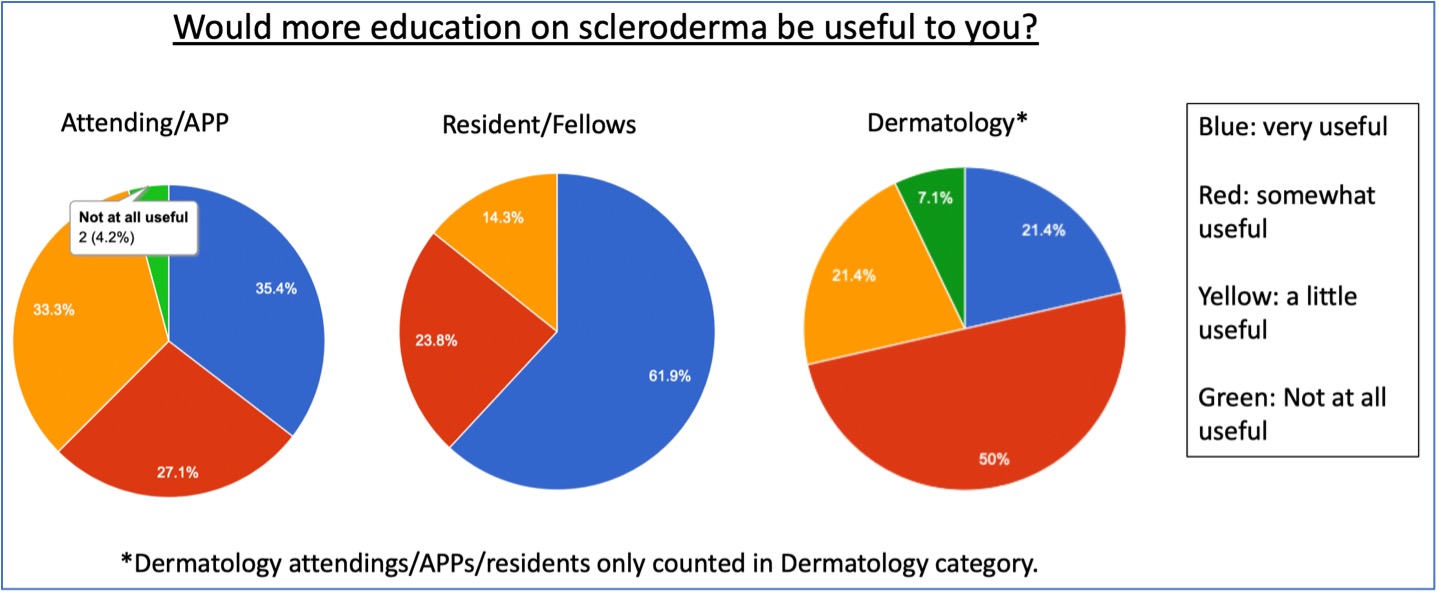 Figure 1: Map representing state origin of survey responses.
Figure 1: Map representing state origin of survey responses.
.jpg) Figure 2: Table depicting aggregate responses to questions related to juvenile localized scleroderma knowledge.
Figure 2: Table depicting aggregate responses to questions related to juvenile localized scleroderma knowledge.
.jpg) Figure 3: Diagram of preferences on additional education on juvenile scleroderma.
Figure 3: Diagram of preferences on additional education on juvenile scleroderma.
To cite this abstract in AMA style:
Guess R, Curran M, Zickuhr L, Moquin R. Targeted Needs Assessment of Provider Medical Knowledge of Juvenile Scleroderma, a Mixed Methods Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/targeted-needs-assessment-of-provider-medical-knowledge-of-juvenile-scleroderma-a-mixed-methods-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/targeted-needs-assessment-of-provider-medical-knowledge-of-juvenile-scleroderma-a-mixed-methods-study/
