Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Up to half of patients who transition to adult care are lost to follow up within 2 years of transfer from pediatric to adult rheumatology (Hart, Clin. Pediatr. 2019; 58 (11-12): 1277-1283). Complicating matters is the lack of training for pediatric and adult specialists in transition, with nearly 50% of adult rheumatologists reporting no transitional care training (Zizman, Arth. Care Res. 2020; 72:432–40) . The goal of this exploratory pilot study is to assess patient independence, transition readiness, understanding of disease and attitudes towards existing transition documents through qualitative interviews. Through input from providers, patients and their parents, we intend to apply human-centered-design to create a single page transfer summary and tools for transition to be incorporated into clinical practice.
Methods: Semi-structured interviews were conducted on rheumatologists, pre and post-transfer young adult patients (aged 14-26 with an established pediatric rheumatic disease diagnosis, with at least two visits with a pediatric or adult rheumatology provider within the last 24 months) and their parents/guardians (Table 1). Open-ended and Likert scale questions were asked regarding topics ranging from independence, transfer readiness, understanding of disease and opinions towards existing medical summaries on Systemic Lupus Erythematosus (SLE), and Juvenile Idiopathic Arthritis (JIA). Themes were analyzed using the Rapid Data Analysis and Reporting (RADaR) approach by 2 independent reviewers (Table 2). Descriptive analysis of exploratory pilot data was done with top-box scoring and median.
Results: Barriers to medical independence included lack of self-transportation, socio-economic factors, inability to self-administer medications, schedule appointments, self-advocate and an unwillingness to take on increased responsibility despite having capability to do so. There was a discrepancy between providers rating of patients’ general independence as compared to medical independence (Table 3).Pediatric clinics were associated with attentiveness, friendly staff, peaceful environment and caring doctors. Adult clinics were associated with fear, lack of insurance coverage, less attention to detail and long wait times. Transfer readiness was facilitated by mentally preparing patients for adult clinic expectations, patients’ ability to self-advocate, attend appointments alone, rapport with adult physician and adult physician’s knowledge of patient.SLE document was useful for physicians’ understanding of patient disease, yet cumbersome for physicians to fill out and difficult for patients to understand. Documents with additional personal patients’ details were deemed useful to build rapport.Limitations include patient population in rural healthcare system as well as small sample size though further interviews are currently in progress.
Conclusion: Through semi-structured interviews we identified key barriers in transition readiness, independence and gained insight on existing transition documents. We intend to apply principles of human centered design to create an improved transition document and transition process.
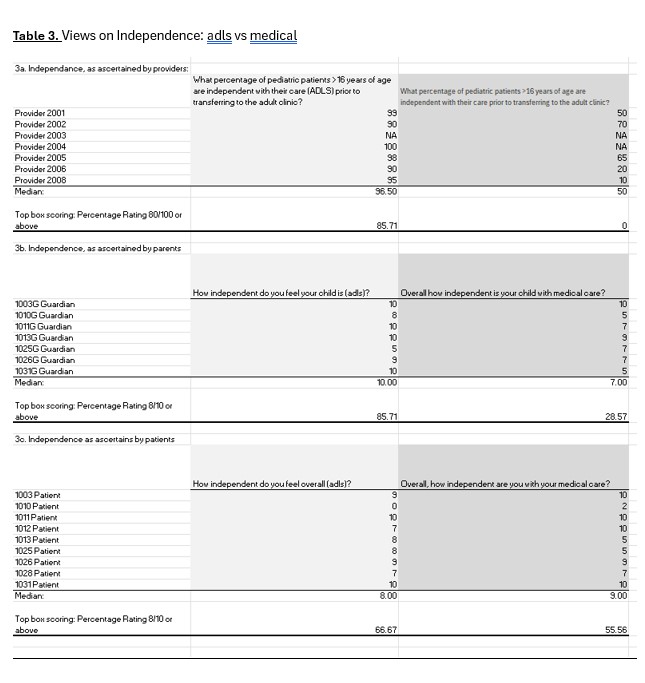 Table 1: Participant Demographics
Table 1: Participant Demographics
.jpg) Table 2: Examples of Abstractions
Table 2: Examples of Abstractions
.jpg) Table 3: Views on Independance: adls vs medical
Table 3: Views on Independance: adls vs medical
To cite this abstract in AMA style:
Chang L, Sharma R, Guziewicz E, Jackson J, Romagnoli K, Campbell G, Korukonda S, Pawar P, Cote J, Davis T, Brunner E. Rheum to Grow:An Approach Towards Human Centered Design through a Qualitative Analysis on the Transition from Pediatric to Adult Rheumatology [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/rheum-to-growan-approach-towards-human-centered-design-through-a-qualitative-analysis-on-the-transition-from-pediatric-to-adult-rheumatology/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheum-to-growan-approach-towards-human-centered-design-through-a-qualitative-analysis-on-the-transition-from-pediatric-to-adult-rheumatology/
