Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile dermatomyositis (JDM) is the most common idiopathic inflammatory myopathy of childhood, characterized by proximal muscle weakness and distinctive cutaneous findings. Magnetic resonance imaging (MRI) has emerged as a valuable, noninvasive diagnostic tool, reducing the reliance on interventional procedures such as muscle biopsy. Myositis-specific antibodies (MSAs) have become important in characterizing disease phenotypes, predicting prognosis, and guiding management strategies. Among these, NXP2 antibodies are associated with a more severe disease course, including higher disease burden, chronicity, and an increased risk of calcinosis. However, although MSA testing may not be as costly as MRI, limited access and specialized processing makes testing potentially challenging, whereas MRI is more routinely accessible in clinical settings. This study aims to evaluate whether pretreatment MRI findings can serve as early predictors of disease phenotype by correlating imaging patterns with MSA status, specifically comparing NXP2-positive and MSA-negative JDM patients.
Methods: With IRB approval, we conducted a retrospective review of NXP2-positive and MSA-negative JDM at Texas Children’s Hospital over the past 10 years. Included patients had at least 1 year of data and initial MRI without prior systemic treatment. All patients met 2017 EULAR/ACR criteria for probable or definite idiopathic inflammatory myopathies. MRI scans of the pelvis and thighs were assessed by a musculoskeletal radiologist blinded to MSA status and clinical outcomes. MRI findings were evaluated using the Ladd et al. scoring tool, focusing on muscle and fascial signal abnormalities and reticulated subcutaneous fat changes. Associations between MRI findings and clinical outcomes, including the Disease Activity Score (DAS)—a validated tool—were analyzed.
Results: Thirty-three patients with JDM met inclusion criteria: 18 NXP2-positive and 15 MSA-negative. Initial MRI scores did not identify significant differences between the two groups. However, when analyzed irrespective of MSA status, pretreatment MRI of the anterior thigh (p < 0.001), adductors (p = 0.006), pelvis (p = 0.006) and fat signal abnormalities (p=0.047) were associated with higher disease activity scores. At six months, NXP2-positive patients continued to exhibit upper, truncal, and neck muscle weakness, though not statistically significant. At two years, they showed persistently elevated muscle enzymes (AST/ALT and aldolase) and a higher prevalence of calcinosis (28% vs. 5.6%). MSA-negative patients had more mucocutaneous features, including Gottron’s papules (93% vs 50%) and heliotrope rash (80% vs 39%).
Conclusion: Pretreatment MRI findings did not differentiate NXP2-positive from MSA-negative JDM. However, abnormalities in subcutaneous fat and specific muscle groups were linked to higher disease activity regardless of antibody status. Limitations include retrospective design, small sample size, and single-center cohort, which may limit the generalizability and statistical power of subgroup comparisons. Larger, multicenter studies are needed to confirm whether initial MRI can serve as a prognostic tool in JDM.
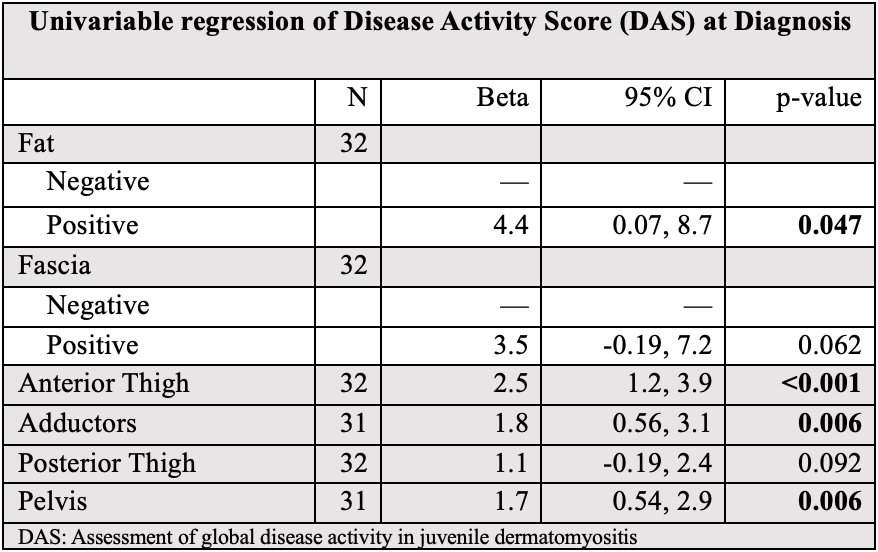 Table 1: Patient Demographics and Clinical Characteristics
Table 1: Patient Demographics and Clinical Characteristics
.jpg) Table 2: MRI Signal Abnormalities by Myositis Specific Antibody
Table 2: MRI Signal Abnormalities by Myositis Specific Antibody
.jpg) Table 3 Univariable Regression MRI findings on the Disease Activity Score at Diagnosis
Table 3 Univariable Regression MRI findings on the Disease Activity Score at Diagnosis
To cite this abstract in AMA style:
Torres Sanchez J, Bawa P, Ramirez A, Nguyen M, Thakral A, Huang X, Kan J, De Guzman M. Initial MRI Findings as Predictors of Disease Phenotype in Juvenile Dermatomyositis: A Comparative Study of Myositis Specific Antibodies NXP2-Positive and Myositis Specific Antibody-Negative Patients in a Large Tertiary Hospital [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/initial-mri-findings-as-predictors-of-disease-phenotype-in-juvenile-dermatomyositis-a-comparative-study-of-myositis-specific-antibodies-nxp2-positive-and-myositis-specific-antibody-negative-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/initial-mri-findings-as-predictors-of-disease-phenotype-in-juvenile-dermatomyositis-a-comparative-study-of-myositis-specific-antibodies-nxp2-positive-and-myositis-specific-antibody-negative-patients/
