Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: A combination of traditional risk factors and chronic inflammation account for the excess cardiovascular risk (CV) observed in rheumatoid arthritis (RA), including atherosclerotic cardiovascular disease (ASCVD) and heart failure (HF). Advanced cardiac imaging methods enable quantitative measurements of CV risk while informing mechanisms for risk such as coronary microvascular disease and plaque burden. The recently published PREVENT equations enable estimates for 10-year risk for ASCVD and HF. The objective of this study was to determine the correlation between the PREVENT estimated ASCVD and HF risk with imaging measurements corresponding to mechanisms of CV risk, specifically coronary microvascular function and plaque volume in patients with RA.
Methods: We studied subjects from the Lipids, Inflammation and Cardiovascular Risk in RA (LiiRA) study (1), which enrolled RA patients, age >35, without a history of CVD, not on a statin and about to initiate a TNFi. All subjects underwent a stress myocardial perfusion PET (cardiac PET) enabling calculation of myocardial flow reserve (MFR) and assessment for coronary microvascular disease (CMD) defined as MFR< 2.5. In a long-term extension study 2+ years post-baseline, a subset of LiiRA subjects with and without MFR< 2.5 had a follow-up cardiac PET and a coronary CT angiogram to quantify plaque volume. ASCVD and HF risk was assessed for all subjects using the PREVENT equations. We tested the baseline cross-sectional correlation between the PREVENT-ASCVD and HF risk with MFR using the Spearman rank correlation test. In the subset of patients with long-term follow-up, we tested the correlation between baseline ASCVD and HF risk with MFR and plaque volume at 2+ years (Figure 1).
Results: We studied n=73 subjects, 82% female, 68% seropositive; the overall cohort had low estimated ASCVD and HF risk (Table 1). At baseline a higher HF risk was cross-sectionally correlated with lower MFR (rs=-0.31, p=0.008); no correlation was observed for the PREVENT ASCVD with MFR. In the long-term extension study, a higher HF risk remained correlated with lower MFR (r= -0.54, p=0.022) as well as higher total and non-calcified plaque volume (Table 2).
Conclusion: RA patients with a higher estimated HF risk at baseline had worse coronary microvascular function, in line with prior studies implicating coronary microvascular disease as a mechanism for HF. After 2+ years, a higher estimated HF risk at baseline correlated with worse coronary microvascular function and a higher plaque burden. These findings suggest that the PREVENT HF equations are a promising approach to identify RA patients should be considered for additional CV screening.(1)Weber et al., JAHA 2024;13(9)
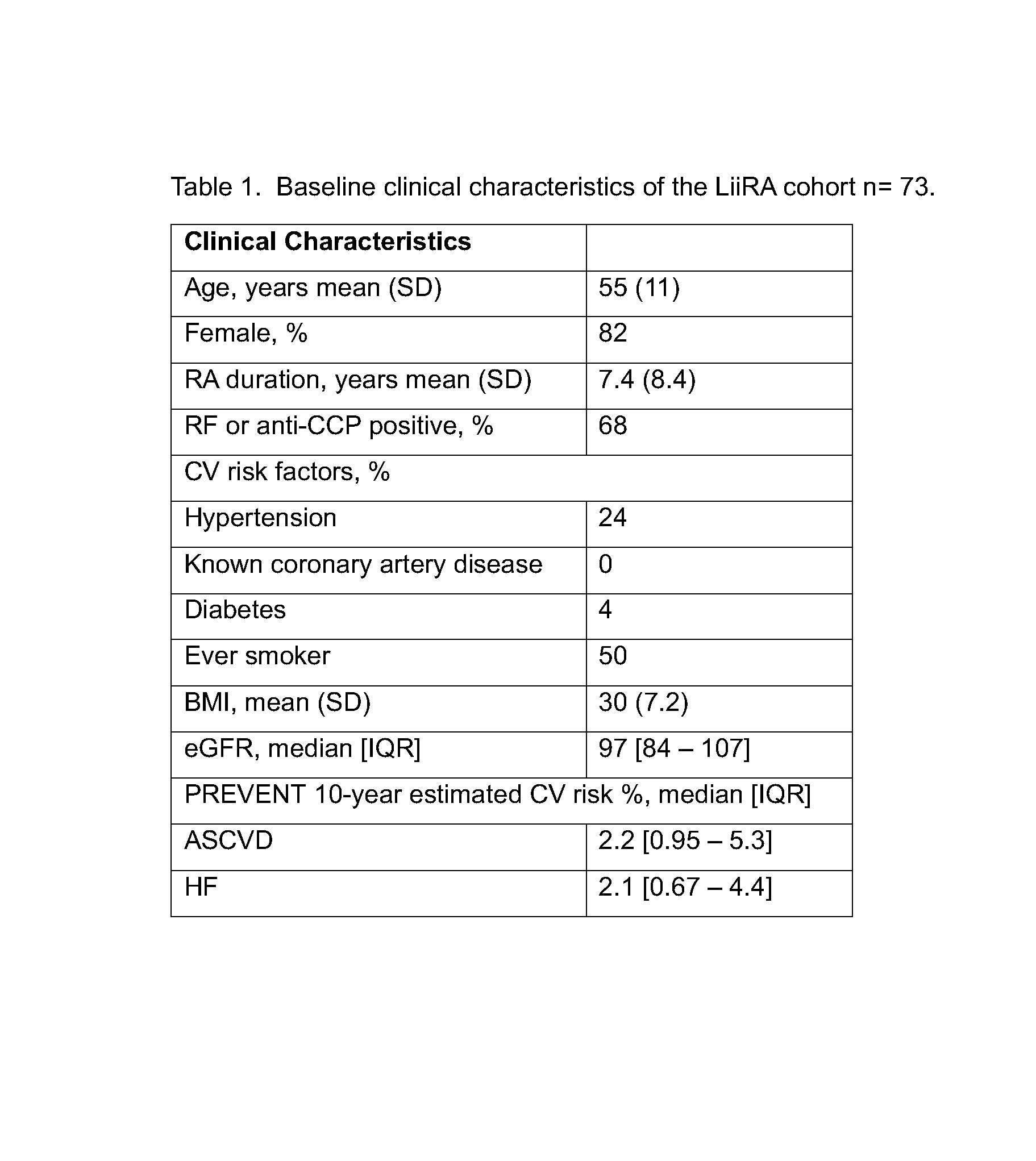 Figure 1. Overview of study design depicting available baseline and follow-up data for analyses.
Figure 1. Overview of study design depicting available baseline and follow-up data for analyses.
.jpg) Table 1. Baseline clinical characteristics of the LiiRA cohort n= 73.
Table 1. Baseline clinical characteristics of the LiiRA cohort n= 73.
.jpg) Table 2. Correlation between baseline PREVENT ASCVD and HF risk with (a) MFR and (b) plaque volume at 2+ years (n=18).
Table 2. Correlation between baseline PREVENT ASCVD and HF risk with (a) MFR and (b) plaque volume at 2+ years (n=18).
To cite this abstract in AMA style:
Zhong K, rusnak L, Qi Y, Usiskin I, McDermott G, Weber B, DiCarli M, Liao K. Correlates Between Cardiovascular Risk Scores with Coronary Microvascular Function and Plaque Burden in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/correlates-between-cardiovascular-risk-scores-with-coronary-microvascular-function-and-plaque-burden-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/correlates-between-cardiovascular-risk-scores-with-coronary-microvascular-function-and-plaque-burden-in-rheumatoid-arthritis/
