Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial Lung Disease (ILD) is a frequent manifestation of Sjögren’s Disease (SjD), associated with significant morbidity and mortality. However, data on the prevalence of progressive ILD in SjD remain scarce, and biomarkers for predicting progression are lacking. Computer-Aided Lung Informatics for Pathology Evaluation and Rating (CALIPER) is a validated CT-based software that quantifies ILD patterns such as ground-glass opacities, reticulation, honeycombing, and low attenuation areas. CALIPER-derived parameters correlate with pulmonary function tests (PFT) and outcomes in IPF and other autoimmune ILDs, but their role in SjD-ILD is unexplored.The aim of this study was to assess the prognostic value of CALIPER-derived parameters in SjD-ILD patients
Methods: SjD patients (2016 ACR/EULAR criteria) with HRCT-confirmed ILD followed from Jan 2018 to Sep 2023 were retrospectively included if ≥1 HRCT was suitable for CALIPER analysis. Clinical, lab, respiratory, and PFT data were collected at baseline and follow-up. Progressive fibrosing ILD (PF-ILD) was defined (ATS criteria) by ≥2 of: worsening symptoms, FVC decline ≥5% or DLCO ≥10%, or radiological progression within 1 year. CALIPER-derived ILD% (sum of ground-glass, reticular, honeycombing) and VRS% (vascular-related structures) were calculated. Visual ILD extent (Warrick score) and ILD pattern were assessed by a thoracic radiologist
Results: Twenty-three patients (F:M=18:5, mean age 66.2±9.5 yrs, mean follow-up 6.1±5 yrs) were enrolled. ILD patterns included NSIP (n=14), UIP (n=6), and NSIP+OP (n=3). Dyspnea and cough occurred in 21 and 19 patients, respectively. Median baseline FVC and DLCO were 83% and 64%. Seventeen patients received immunosuppressants; none received antifibrotics. Seven required long-term oxygen (LTO2) and 7 developed PF-ILD. Both baseline ILD% and VRS% demonstrated a moderate to strong correlation with FCV% and DLCO%, visual ILD quantification with Warrick score and between them (table 1). VRS%, Reticulation%, and Honeycombing% were significantly higher in UIP (p=.021, .038, and .047, respectively). On univariate regression analysis, VRS% (OR 3.2, 95%CI 1.1-9.1, p=.03) and ILD% (OR 1.13, 95%CI 1.01-1.3, p=.05) were associated with LTO2 necessity. According to ROC analysis, VRS% had an AUC of 0.813 (p=.019) with an optimal cut-off of 3.8%, yielding a sensitivity of 71.4% and a specificity of 87.5% in predicting LTO2 necessity. ILD% had an AUC of 0.777 (p=.038) with a cut-off of 11.6% resulting in a sensitivity of 71.4% and a specificity of 75% in predicting LTO2 necessity.On univariate regression analysis VRS% (OR 2.8, 95%CI 1-8, p=.05) was associated with a PF-ILD behavior in the next year, with an AUC of 0.85 (p=.023) and an optimal cut-off of 3.8% resulting in a sensitivity of 83.3% and specificity of 80%.
Conclusion: CALIPER-derived parameters correlate strongly with lung function and predict adverse outcomes in SjD-ILD. Automated HRCT analysis offers promising digital biomarkers for disease assessment and risk stratification. Integrating these metrics with clinical and functional data could support early identification of progressive ILD and guide therapy. Further validation in larger cohorts is warranted
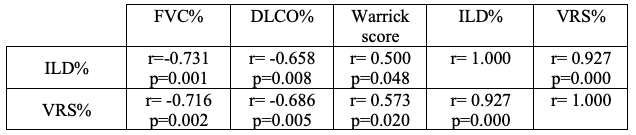 Correlation of CALIPER-derived parameters with functional indices and HRCT visual assessment with Warrick score
Correlation of CALIPER-derived parameters with functional indices and HRCT visual assessment with Warrick score
To cite this abstract in AMA style:
La Rocca G, Ferro F, Uggenti V, Dei B, Fulvio G, Moretti M, Mosca M, Romei C, Baldini C. Quantitative HRCT Analysis in Sjögren’s Disease-associated ILD: CALIPER-Derived Imaging Biomarkers for Prognostic Assessment [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/quantitative-hrct-analysis-in-sjogrens-disease-associated-ild-caliper-derived-imaging-biomarkers-for-prognostic-assessment/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/quantitative-hrct-analysis-in-sjogrens-disease-associated-ild-caliper-derived-imaging-biomarkers-for-prognostic-assessment/
