Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Knee osteoarthritis (OA) is a leading cause of functional limitation (FL) in older adults. As there is no cure, treatment centers around symptom management, with physical activity (PA) being strongly recommended. PA is beneficial for those with knee OA, as participation in more moderate-to-vigorous physical activity (MVPA) reduces risk of FL. Sufficient sleep is necessary for adequate recovery of the musculoskeletal system; however, it is unknown if sleep quality changes the relationship between PA and OA-related outcomes. Therefore, the purpose of this study was to investigate if sleep quality modifies the relationship between PA and FL in adults with or at high risk for knee OA.
Methods: We used data from the Osteoarthritis Initiative (OAI). Our exposure was min/week of MVPA, collected at the 48-month visit (analytic baseline, BL) using an Actigraph GT1M monitor. Participants were dichotomized as meeting or not meeting PA Guidelines (≥ 150 vs < 150 min/week of MVPA). Our outcome was incident FL, collected at BL and 4 years later (96-month visit). FL was defined as walking < 1.22 m/s on a 20m self-selected walking speed assessment. Sleep quality was assessed from a question asking participants to rate how often their sleep was restless in the past week from the Center for Epidemiologic Studies Depression Scale (CES-D), collected at BL. Participants were dichotomized as having good sleep quality (< 1 day of restless sleep) vs poor sleep quality (≥ 1 day of restless sleep). Risk ratios (RR) with 95% confidence intervals (CI) were calculated using log-binomial regression to determine the associations between PA and incident FL. To determine if sleep quality was an effect measure modifier, these analyses were repeated in separate models stratified by sleep quality.
Results: 1126 participants (age = 62.9 years old, 51% female, BMI =28.5 kg/m2) were included in the analytic sample. 234 participants (20.8%) developed FL 4 years later. Overall, participants who met PA guidelines had a 32% decreased risk of incident FL compared to participants who did not meet PA guidelines (adjusted RR [95% CI] = 0.68 [0.48, 0.98]). For participants with good sleep quality, those who met PA guidelines had a 45% decreased risk of incident FL compared to those who did not meet PA guidelines (adjusted RR [95% CI] = 0.55 [0.18, 0.50]). For participants with poor sleep quality, this decreased risk of incident FL was attenuated for those meeting PA guidelines and did not meet statistical significance (adjusted RR [95% CI] = 0.81 [0.51, 1.30]).
Conclusion: Sleep quality appears to modify the relationship between PA and FL such that only those with good sleep benefit from meeting PA guidelines. However, more research is needed to determine if sleep quality truly represents a physiological modifier of the body’s response to PA or is simply a marker of underlying health and not directly in the causal pathway.
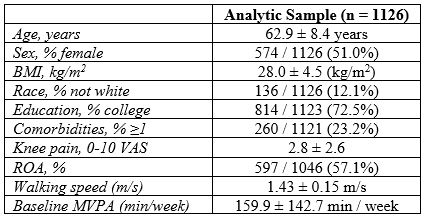 Table 1: Baseline demographics for the analytic sample
Table 1: Baseline demographics for the analytic sample
.jpg) Table 2: Risk ratios (RR) and 95% confidence intervals (95% CI) for incident functional limitation by MVPA level, stratified by sleep quality
Table 2: Risk ratios (RR) and 95% confidence intervals (95% CI) for incident functional limitation by MVPA level, stratified by sleep quality
To cite this abstract in AMA style:
Jakiela J, Acosta G, Lucas D, Moser M, Whitted C, Liles S, White D. Sleep Quality as a Modifier of the Relationship Between Physical Activity and Functional Limitation in Adults with or at High Risk of Knee Osteoarthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/sleep-quality-as-a-modifier-of-the-relationship-between-physical-activity-and-functional-limitation-in-adults-with-or-at-high-risk-of-knee-osteoarthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sleep-quality-as-a-modifier-of-the-relationship-between-physical-activity-and-functional-limitation-in-adults-with-or-at-high-risk-of-knee-osteoarthritis/
