Session Information
Date: Monday, October 27, 2025
Title: (1553–1591) Systemic Sclerosis & Related Disorders – Clinical Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is the main cause of mortality in systemic sclerosis (SSc). Among radiomics features, the automated quantification of pulmonary vascular volume (PVV) on high-resolution computed tomography (HRCT) was predictive of survival and functional changes in idiopathic pulmonary fibrosis (IPF) and rheumatoid arthritis (RA)-associated ILD (Jacob, 2018). In SSc, PVV was associated with ILD severity (extent on HRCT, pulmonary function tests values: pFVC%, pDLCO%). Here, we explored the predictive value of CT-derived radiomics features for mortality and ILD progression in SSc-ILD.
Methods: We included SSc patients from a single referral centre with ILD present on HRCT and at least one follow-up visit. The progression analysis focused on patients with lung function repeated within 12±3 months. ILD progression was defined as at least one of the following:FVC relative decline ≥ 10 %FVC relative decline ≥ 10 % or FVC 5-9% and DLCO relative decline ≥ 15%FVC absolute decline ≥ 5%FVC absolute decline ≥ 5 or DLCO absolute decline ≥ 10%HRCT scans underwent lung texture analysis (LTA, Imbio). The percentage distribution of ground-glass, reticular, honeycombing (the latter two defining “fibrotic alterations”), hyperlucency, normal lung and PVV was quantified in upper, middle and lower zones and the whole lung. Survival analysis was performed from the first ILD-positive CT until last contact (death or alive status), using Cox proportional hazards models, with radiomics parameters adjusted for the SCOpE score (Elhai, 2017). Radiomics predictors of ILD progression were assessed using the logistic Generalized Estimating Equations (GEE), adjusted for established risk factors.
Results: Among 267 SSc-ILD patients, 65 (24%) deaths were recorded over a median follow up of 42 (27-110) months. Patients who died were older, clinically and functionally more severely impaired (Table I) and with higher extent of PVV% and parenchymal alterations in all lung zones (Table II). In a multivariable Cox model, the PVV% of the upper zones (HR 1.28, 95% CI 1.12-1.47) and the SCOpE score (HR 1.22, 95% CI 1.15-1.28) independently predicted mortality (Fig IA).Among the 261 yearly follow-ups from 160 SSc-ILD patients, we recorded 99 episodes of ILD progression (38%), occurring in 64 patients (40%). Patients with progressive ILD had more frequently increased inflammatory markers, better-preserved pulmonary function tests (Table I), but comparable radiomics changes versus non-progressors (Table II). In a multivariable model integrating clinical and radiomics predictors selected through univariable analysis, only pDLCO% (OR 1.02, 95% CI 1.01-1.04) and pFVC% (OR 1.03, 95% CI 1.01-1.05) were independently associated with ILD progression (Fig IB). Comparable results were obtained when each progression definition was analysed separately.
Conclusion: In line withRA-ILD and IPF, PVV% of the upper zones significantly predicts mortality in SSc-ILD. Conversely, we could not detect radiomics predictors for ILD progression. Further studies are needed to support the identification of patients at risk of ILD progression and prompt therapeutic interventions.
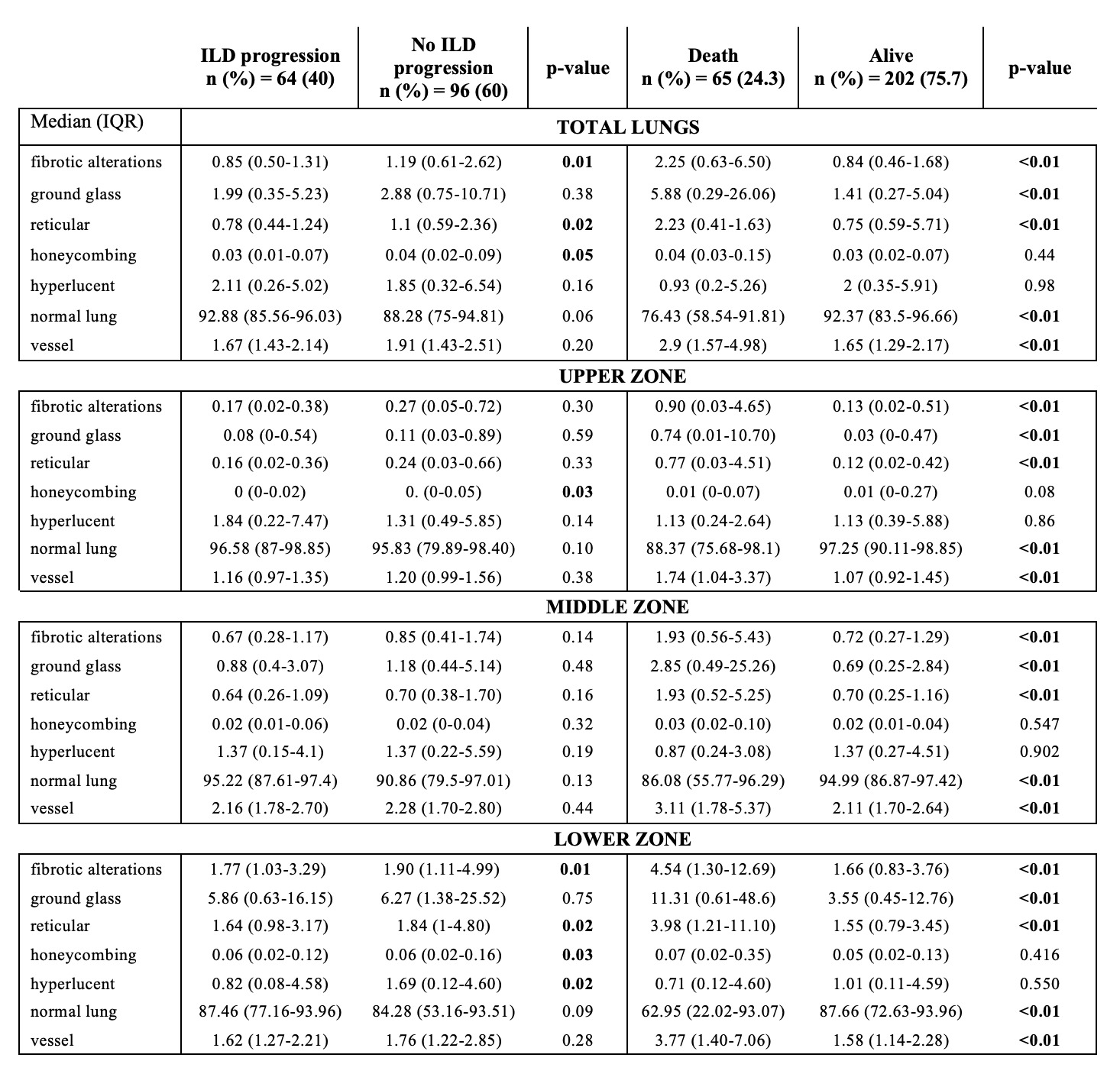 Table I. Clinical and functional characteristics of the study population.
Table I. Clinical and functional characteristics of the study population.
ACA: anti-centromere antibodies; ATA: anti-topoisomerase I antibodies; ARA: anti-RNA polymerase III antibodies; antiPm-Scl: anti-PM-scleroderma-antibodies; dcSSc: diffuse cutaneous systemic sclerosis; NVC: nailfold videocapillaroscopy; NYHA: New York Hearth Association; pFVC%: predicted forced vital capacity; pDLCO/SB%: predicted diffusion of the lung for carbon monoxide on single breath; 6MWT: 6 minutes walking test
Increased inflammatory markers defined as ESR or/and CRP above normal levels
.jpg) Table II. Distribution of radiomics parameters in the total lungs among systemic sclerosis patients with progressive disease or death
Table II. Distribution of radiomics parameters in the total lungs among systemic sclerosis patients with progressive disease or death
Fibrotic alterations = reticular pattern + honeycombing
.jpg) Fig I. Forrest plot showing predictive radiomics and clinical risk factors for mortality (IA) and progression (IB).
Fig I. Forrest plot showing predictive radiomics and clinical risk factors for mortality (IA) and progression (IB).
To cite this abstract in AMA style:
Iacovantuono M, landini N, Jungblut l, Käs F, Dobrota R, Muraru S, Mihai C, Elhai M, Becker M, Chimenti M, Frauenfelder T, Hoffmann-Vold A, Distler O, Bruni C. Exploring the Pulmonary Vascular Changes on Computed Tomography in predicting progression and mortality of Systemic Sclerosis-associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/exploring-the-pulmonary-vascular-changes-on-computed-tomography-in-predicting-progression-and-mortality-of-systemic-sclerosis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exploring-the-pulmonary-vascular-changes-on-computed-tomography-in-predicting-progression-and-mortality-of-systemic-sclerosis-associated-interstitial-lung-disease/
