Session Information
Date: Monday, October 27, 2025
Title: (1553–1591) Systemic Sclerosis & Related Disorders – Clinical Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Gastric antral vascular ectasia (GAVE), commonly known as “watermelon stomach,” is a rare but potentially severe gastrointestinal manifestation in systemic sclerosis (SSc). Despite its known association with SSc, data regarding demographic patterns, comorbidity profiles, and inpatient mortality among this subset remain limited. This study aimed to analyze the factors associated with GAVE in hospitalized SSc patients, including age, sex, comorbidities, and mortality, using a national inpatient dataset.
Methods: A retrospective cohort study was conducted using an extensive national inpatient database to identify patients with scleroderma, stratifying them by the presence or absence of GAVE. Patient demographics, comorbidities, and inpatient mortality were compared using logistic regression and descriptive statistics. Odds ratios (ORs), standard errors, 95% confidence intervals (CIs), and p-values were reported to assess statistical significance.
Results: Among 152,971 hospitalized SSc patients, 24,451 (1.62%) had a diagnosis of GAVE. Patients with GAVE were older (mean age 68.9 vs. 63.4) and predominantly female. There were no statistically significant sex-based differences in GAVE prevalence (p=0.7498), but racial differences were significant (p=0.0002), with White and Asian patients more commonly affected. Several comorbidities were significantly associated with GAVE in SSc, including chronic kidney disease (CKD) (p=0.0000), coronary artery disease (p=0.0000), heart failure (p=0.0000), pulmonary fibrosis (p=0.0064), and GERD (p=0.0025). Logistic regression for inpatient mortality in SSc patients revealed increasing age was a significant risk factor (OR 1.01, CI 1.01–1.02, p< 0.001). Male sex (OR 1.35) and African American race did not significantly impact mortality. AKI (OR 4.1), CKD (OR 1.56), heart failure (OR 2.28), myocarditis (OR 2.4), pulmonary hypertension (OR 1.7), and pulmonary fibrosis (OR 1.6) were all independently associated with increased inpatient mortality. Interestingly, obesity (OR 0.7), hypertension (OR 0.5), and GERD (OR 0.58) appeared to be protective. GAVE itself was not significantly associated with mortality (OR 0.9, CI 0.58–1.4, p=0.65).
Conclusion: This national inpatient analysis highlights significant demographic and comorbidity trends in SSc patients with GAVE. While GAVE is associated with distinct clinical features and comorbidities, it was not independently linked to an increase in inpatient mortality. Instead, traditional predictors such as AKI, heart failure, and pulmonary complications played a more prominent role in poor outcomes. Understanding these patterns may guide risk stratification and improve multidisciplinary care strategies in scleroderma.
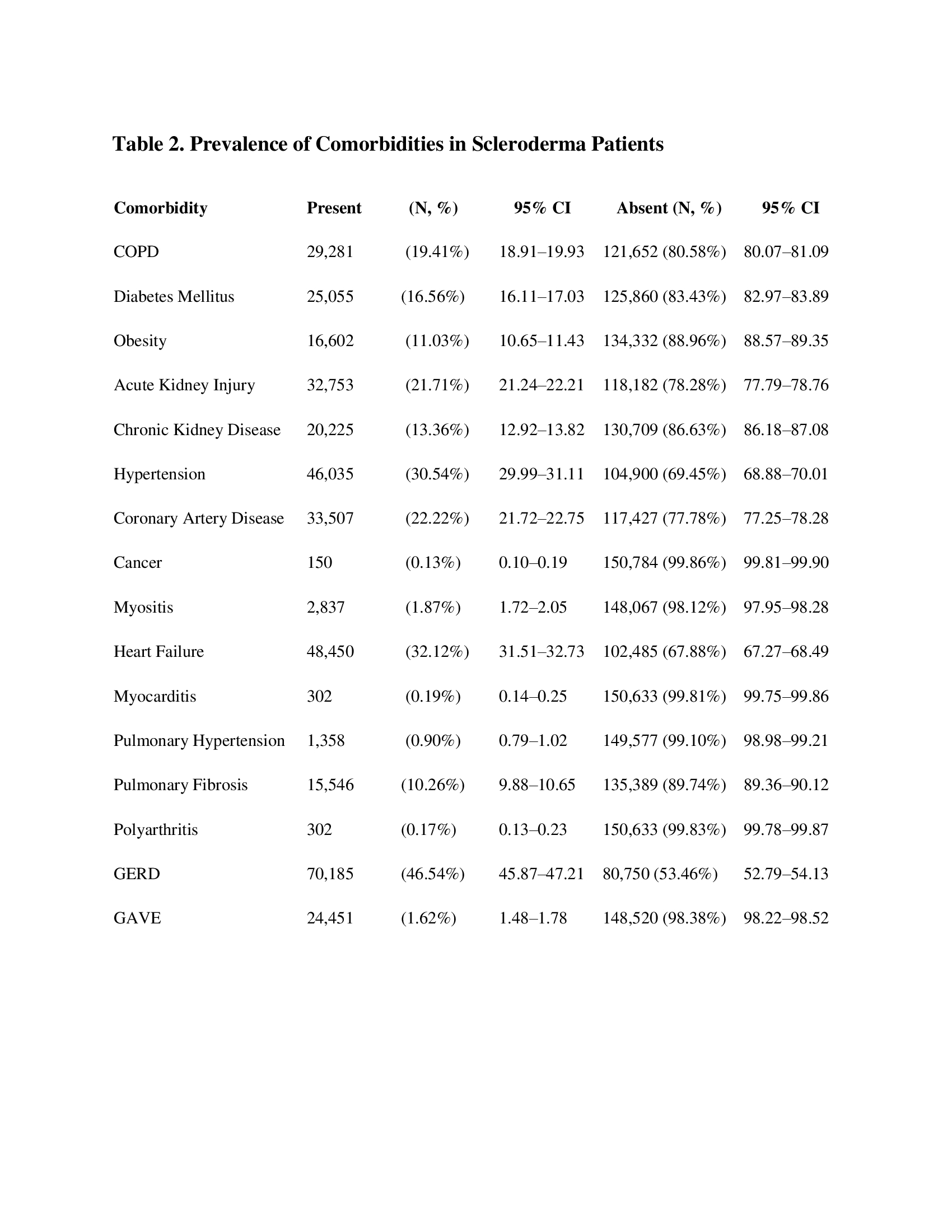 Table 1. Logistic Regression of In-Hospital Mortality in Scleroderma Patients
Table 1. Logistic Regression of In-Hospital Mortality in Scleroderma Patients
.jpg) Table 2. Prevalence of Comorbidities in Scleroderma Patients
Table 2. Prevalence of Comorbidities in Scleroderma Patients
Table 3. Comparison of Scleroderma Patients With and Without GAVE
To cite this abstract in AMA style:
Sharma A, Kurra V, Mehta N. Demographic, Clinical, and Mortality Trends in Scleroderma Patients with Gastric Antral Vascular Ectasia (GAVE): A National Inpatient Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/demographic-clinical-and-mortality-trends-in-scleroderma-patients-with-gastric-antral-vascular-ectasia-gave-a-national-inpatient-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/demographic-clinical-and-mortality-trends-in-scleroderma-patients-with-gastric-antral-vascular-ectasia-gave-a-national-inpatient-analysis/

.jpg)