Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease with heterogeneous hematologic manifestations. Thrombocytopenia (TP) in SLE may be associated with major organ involvement and poor prognosis. In this study, we aimed to evaluate the frequency and prognostic significance of TP in a large, multi-center, real-world SLE cohort.
Methods: We conducted a retrospective cohort study using the TriNetX Research Network, a de-identified, federated electronic health record database (accessed March 20, 2025). Adult patients (≥18 years) with SLE (ICD-10: M32.9) and TP (ICD-10: D69.6), with at least one follow-up encounter, were included. A 1:1 propensity score matching was performed using 41 variables including demographics, comorbidities, and medication exposures to balance baseline characteristics. Continuous and categorical variables were compared using t-tests and chi-squared tests (α = 0.05).
Results: A total of 17,407 patients with SLE and TP (SLE-TP) and 118,640 without TP (SLE-non-TP) were identified, with SLE-TP comprising 14.7% of the cohort. Before matching, SLE-TP patients were more likely to be male and African American (p < 0.001) and had significantly higher frequencies of inflammatory arthritis, pleurisy, glomerular disease, antiphospholipid syndrome, seizure, and hemolytic anemia (all p < 0.05). Comorbidities including obesity, type 2 diabetes, and hypertension were also more common in the SLE-TP group (all p < 0.001) After matching, African American patients were slightly less prevalent in the SLE-TP group compared to the SLE-non-TP group (29.3% vs. 30.7%, p = 0.005). SLE-TP patients had significantly higher rates of peripheral neuropathy (p = 0.006), La/SSB autoantibody (p = 0.013), low C3 (p = 0.001), and low C4 (p < 0.001) (Table 1 and Table 2). There was a trend toward higher obesity in the SLE-TP group (p = 0.093). Use of immunosuppressive medications was not significantly different between the matched groups (Table 2).During the study period, 3,182 (18.6%) SLE-TP patients and 1,368 (8.0%) SLE-non-TP patients died (relative risk [RR]: 2.33; 95% CI: 2.19–2.47) (Figure 1A). Survival analysis showed significantly worse prognosis in the SLE-TP group (hazard ratio [HR]: 1.94; 95% CI: 1.83–2.07; p < 0.001) (Figure 1B), indicating that SLE patients who had thrombocytopenia exhibited a significantly lower survival probability compared to those without this condition.
Conclusion: The presence of La/SSB autoantibody, hypocomplementemia (low C3 and C4), and peripheral neuropathy are the immunological and clinical features most strongly associated with SLE-TP. More importantly, this group faces over a twofold increase in mortality with survival analysis confirming a significantly worse prognosis. These findings confirm thrombocytopenia as a powerful prognostic marker in SLE, indicating that low platelet counts are linked to substantially worse outcomes and nearly double the risk of death.
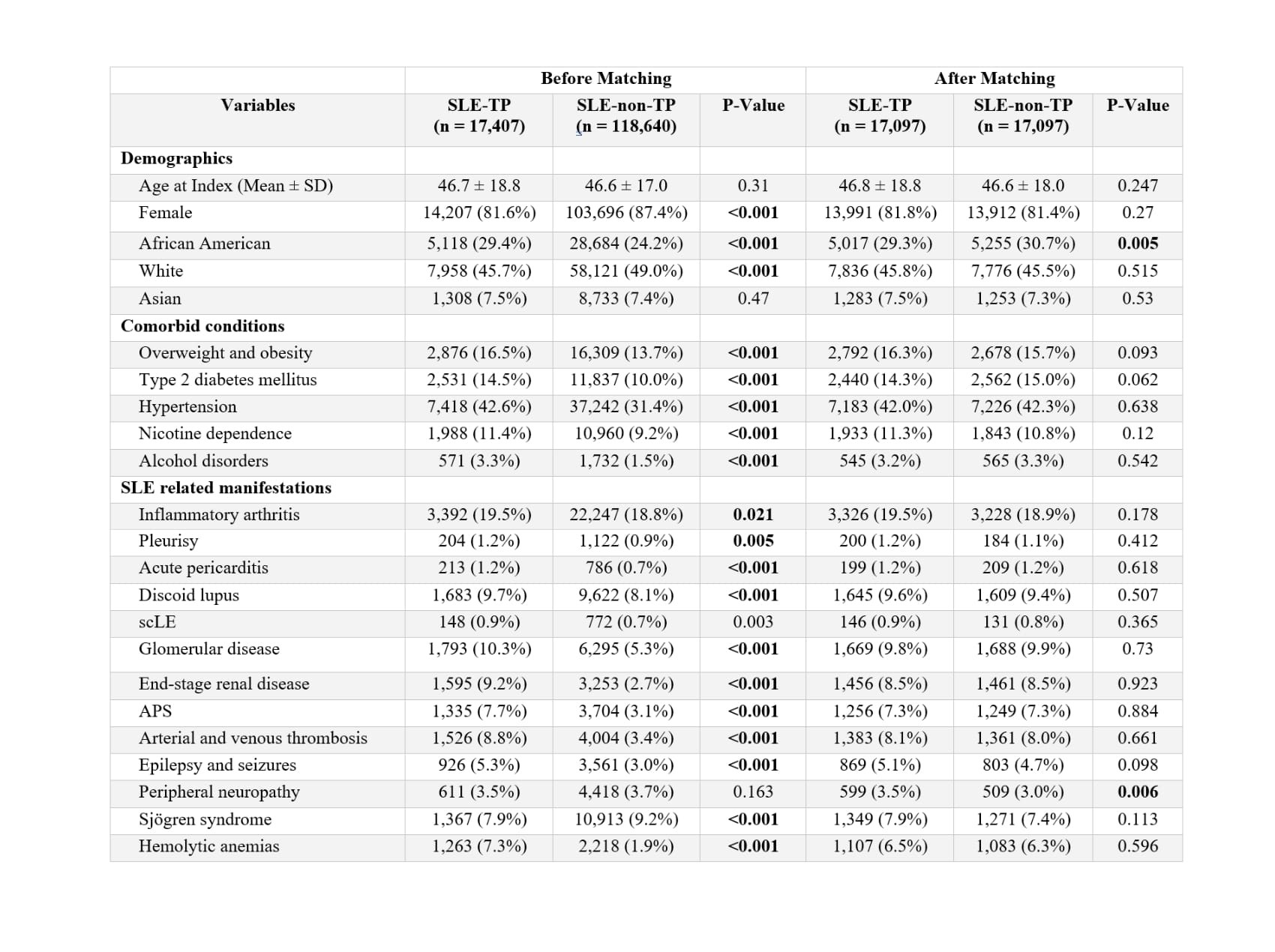 Table 1: Baseline characteristics and comorbidities in patients with SLE with and without thrombocytopenia before and after propensity score matching.
Table 1: Baseline characteristics and comorbidities in patients with SLE with and without thrombocytopenia before and after propensity score matching.
.jpg) Table 2: Serologic profile and immunosuppressive medication use in SLE patients with and without thrombocytopenia before and after propensity score matching.
Table 2: Serologic profile and immunosuppressive medication use in SLE patients with and without thrombocytopenia before and after propensity score matching.
.jpg) Figure 1: Impact of thrombocytopenia in SLE on mortality and survival in patients with and without thrombocytopenia.
Figure 1: Impact of thrombocytopenia in SLE on mortality and survival in patients with and without thrombocytopenia.
To cite this abstract in AMA style:
Heydari-Kamjani M, Daneshvar A, Guan C, Harper E, Pfeil K, Frumker L, Gump M, Pamuk O. Thrombocytopenia in SLE: A Hidden Prognostic Marker of Increased Mortality and Adverse Outcomes – Results from Real World Data [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/thrombocytopenia-in-sle-a-hidden-prognostic-marker-of-increased-mortality-and-adverse-outcomes-results-from-real-world-data/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/thrombocytopenia-in-sle-a-hidden-prognostic-marker-of-increased-mortality-and-adverse-outcomes-results-from-real-world-data/
