Session Information
Date: Monday, October 27, 2025
Title: (1306–1346) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Endogenous estrogens associate with cardioprotective benefits in the general population. Yet, dual pro- and anti-inflammatory effects were described in autoimmune states depending on concentration, disease entity and stage, cell-type involved, target organ environment, and intracellular metabolism. We here explore associations between endogenous estrogens, coronary atherosclerosis and cardiovascular risk in patients with rheumatoid arthritis (RA). Since RA activity is higher in females, especially after menopause, and inflammation is linked to cardiovascular risk, we interrogated whether these relationships varied by sex and menopause and whether they reflected differences in inflammation and lipoprotein functions influencing cell cholesterol homeostasis.
Methods: Computed tomography angiography evaluated coronary atherosclerosis in 140 patients without known cardiovascular disease from a single-center. Serum estrone and 17-b-estradiol were measured with Elisa. Serum cholesterol loading capacity (CLC) on macrophages, which enhances atherosclerosis, was measured in THP-1 monocyte-derived macrophages. High-density lipoprotein cholesterol efflux capacity from macrophages via ATP-binding-cassette-A1 (ABCA1-CEC) and G1 transporters (ABCG1-CEC), which attenuates atherogenesis, was assessed in J774 macrophages and Chinese hamster ovary cells.
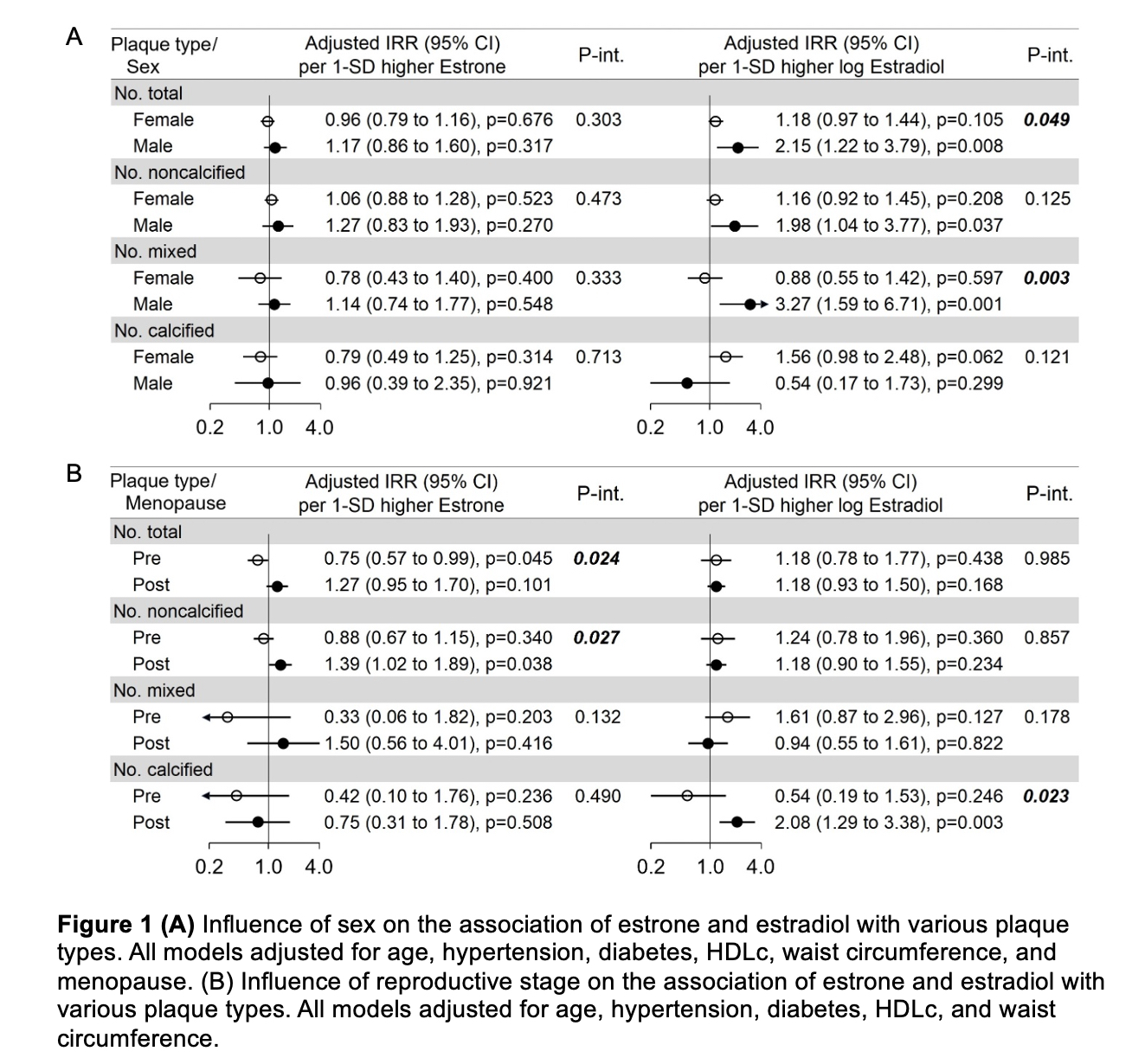
Results: Estrone and estradiol associated with higher coronary artery calcium score (p for interaction 0.023) and estradiol with more coronary plaques (p-for-interaction 0.048) in males but not females. Estrone was linked to fewer plaques in premenopausal women (p for interaction 0.043), while both estrone and estradiol associated with more plaques in postmenopausal women (Figure 1A and B). Estrone associated with higher proatherogenic cytokine levels in males (Figure 2A) and in postmenopausal women, but lower levels in premenopausal women (Figure 3A). Likewise, estrone inversely associated with ABCA1-CEC (p-for-interaction 0.008) and ABCG1-CEC (p for interaction 0.040) in males (Figure 2B and 3B), while estradiol positively associated with CLC (p for interaction 0.044) and inversely with ABCA1-CEC (p-for-interaction 0.010) in males. Estrone, but not estradiol, inversely associated with cardiovascular risk (adjusted hazards ratio 0.43 [95% confidence interval 0.21-0.86] per standard deviation increase), particularly among premenopausal women (p for interaction=0.015).
Conclusion: Sex and reproductive status modified the effect of endogenous estrogens on coronary atherosclerosis in RA and their associations with inflammation and lipoprotein functions impacting on cholesterol homeostasis. Importantly, estrone levels inversely associated with cardiovascular risk independently of ASCVD score and coronary plaque burden, and further optimized risk estimates.
To cite this abstract in AMA style:
Karpouzas G, Papotti B, Ormseth S, Palumbo M, Budoff M, Ronda N. Sex and reproductive stage modify the role of endogenous estrogens on coronary atherosclerosis in rheumatoid arthritis and differences reflect effects on inflammation and cholesterol metabolism [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/sex-and-reproductive-stage-modify-the-role-of-endogenous-estrogens-on-coronary-atherosclerosis-in-rheumatoid-arthritis-and-differences-reflect-effects-on-inflammation-and-cholesterol-metabolism/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-and-reproductive-stage-modify-the-role-of-endogenous-estrogens-on-coronary-atherosclerosis-in-rheumatoid-arthritis-and-differences-reflect-effects-on-inflammation-and-cholesterol-metabolism/

.jpg)
.jpg)