Session Information
Date: Monday, October 27, 2025
Title: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Calcinosis is a feature seen in systemic sclerosis (SSc) and dermatomyositis (DM) that leads to significant morbidity and poor quality of life. Inflammatory vasculopathy is hypothesized to play a role in dystrophic mineral deposition. Paraoxonase1 (PON1) is a high-density lipoprotein (HDL) associated protein that protects the vascular endothelium from oxidative injury and damage. The current study aims to assess the association of calcinosis PON1 activity in SSc and DM patients.
Methods: Calcinosis is a feature seen in systemic sclerosis (SSc) and dermatomyositis (DM) that leads to significant morbidity and poor quality of life. Inflammatory vasculopathy is hypothesized to play a role in dystrophic mineral deposition. Paraoxonase1 (PON1) is a high-density lipoprotein (HDL) associated protein that protects the vascular endothelium from oxidative injury and damage. The current study aims to assess the association of calcinosis PON1 activity in SSc and DM patients.
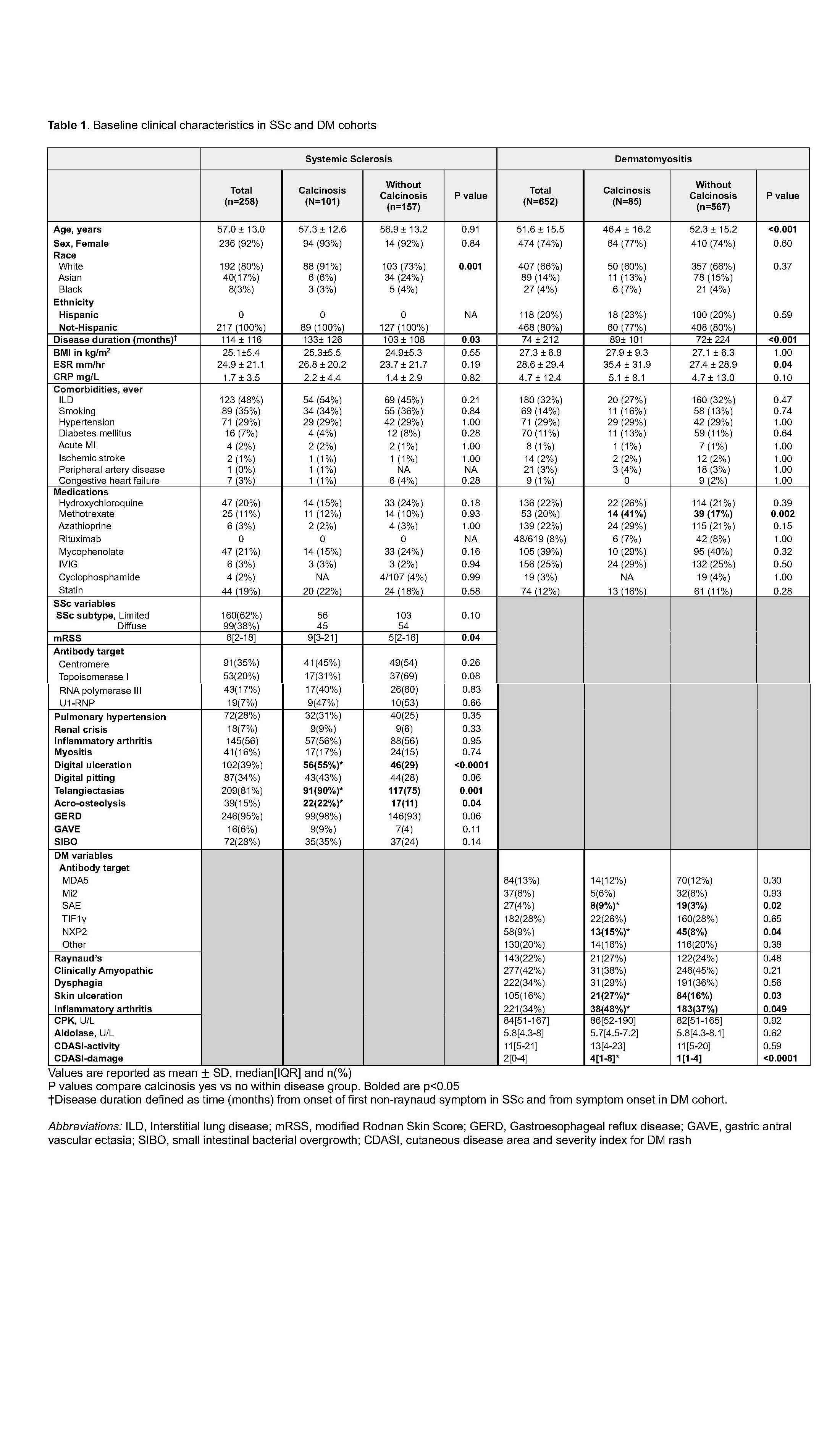
Results: Among 258 SSc patients and 652 DM patients, we identified a total of 186(20%) patients who ever had calcinosis. Calcinosis was more common in SSc (39.6%) compared to DM (13%, p< 0.0001). Calcinosis was associated with longer disease duration in both SSc and DM (Table 1). In SSc, patients with calcinosis were more often white and had higher skin scores, while DM patients with calcinosis were significantly younger, had higher sedimentation rate and had higher incidence of anti SAE and NXP2 antibodies compared to DM without calcinosis (Table 1). Clinical manifestations associated with calcinosis in SSc were digital ulcerations, telangiectasias, and acro-osteolysis, while in DM associated factors were skin ulcers and inflammatory arthritis. PON1 paraoxonase activity was significantly lower in SSc patients with calcinosis compared to SSc without calcinosis, and a similar trend was seen within each DM cohort (Figure 1-a). Association between calcinosis and low PON1 was significant when the two DM cohorts were combined (Figure 1-b). Multivariate models adjusting for age, sex and disease duration demonstrated that the association between low paraoxonase and calcinosis was significant in SSc, in DM total (DM1+DM2) and in all 3 cohorts combined (SSc+DM1+DM2) (Table 2). SSc patients overall had a significantly lower paraoxonase activity compared to DM (p=0.0002), and SSc patients with calcinosis had the lowest paraoxonase activity.
Conclusion: In our current work, calcinosis was observed in 40% of SSc and 13% of DM patients. Calcinosis was associated with longer disease duration and ulcerations in both SSc and DM. Impairment in the activity of the PON1 enzyme, which normally protects the vascular endothelium from oxidative injury, was associated with the presence of calcinosis in both DM and SSc patients, suggesting potential involvement in the disease pathogenesis.
To cite this abstract in AMA style:
Bae S, Davuluri S, Lee B, Lim S, Markovic D, Chung L, Fiorentino D, Charles-Schoeman C. Association of Paraoxonase1 activity with Calcinosis in Patients with Scleroderma and Dermatomyositis : An exploratory analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-of-paraoxonase1-activity-with-calcinosis-in-patients-with-scleroderma-and-dermatomyositis-an-exploratory-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-paraoxonase1-activity-with-calcinosis-in-patients-with-scleroderma-and-dermatomyositis-an-exploratory-analysis/

.jpg)
.jpg)