Session Information
Date: Monday, October 27, 2025
Title: (1147–1190) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: The associations between various myositis-specific antibodies (MSAs), rapidly progressive interstitial lung disease (RP-ILD), and mortality in antisynthetase syndrome (ASS) have been previously reported in several studies, although limited by small sample sizes. RP-ILD has been recognized as a major risk factor for increased mortality in ASS. This study aimed to systematically assess MSAs and clinical factors associated with RP-ILD and mortality in ASS.
Methods: We conducted a systematic review and meta-analysis of cohorts identified through PubMed, MEDLINE, Embase, and Scopus. Studies enrolling individuals with ASS and evaluating risk factors for RP-ILD and mortality were included from inception to December 2024. The primary outcomes were the incidence of RP-ILD and mortality. Pooled risk ratio (RR) and 95% confidence interval (CI) were calculated using a random-effect, generic inverse variance method of DerSimonian and Laird.
Results: A total of 19 studies comprising 1,971 patients were included, with 17 studies analyzed for mortality and 5 for RP-ILD. Random-effects meta-analysis revealed that factors associated with increased mortality included age over 50 years (risk ratio [RR], 2.86; 95% confidence interval [CI], 1.50–5.43; I² = 0%), with a mean difference (MD) of 7.74 years (95% CI, 4.15–11.34), male sex (RR, 1.44; 95% CI, 1.01–2.05; I² = 0%), malignancy (RR, 7.59; 95% CI, 3.87–14.30; I² = 0%), RP-ILD (RR, 4.90; 95% CI, 1.84–13.08; I² = 0%), anti-OJ antibody positivity (RR, 3.03; 95% CI, 2.19–4.18; I² = 0%), and anti-PL7 antibody positivity (RR, 1.65; 95% CI, 1.16–2.35; I² = 0%). Only anti-Ro52 antibody positivity was associated with an increased risk of RP-ILD (RR, 2.75; 95% CI, 1.18–6.40; I² = 38%), with moderate heterogeneity. RP-ILD and mortality were observed in 33.3% and 16.3% of the pooled cohort, respectively.
Conclusion: Anti-Ro52 antibody positivity was significantly associated with RP-ILD in ASS. Increased mortality was associated with age over 50 years, male sex, malignancy, RP-ILD, and positivity for anti-OJ and anti-PL7 antibodies. These findings highlight the potential role of MSAs in stratifying disease severity in ASS. However, given the limited number of studies and observed heterogeneity, these results should be interpreted with caution.
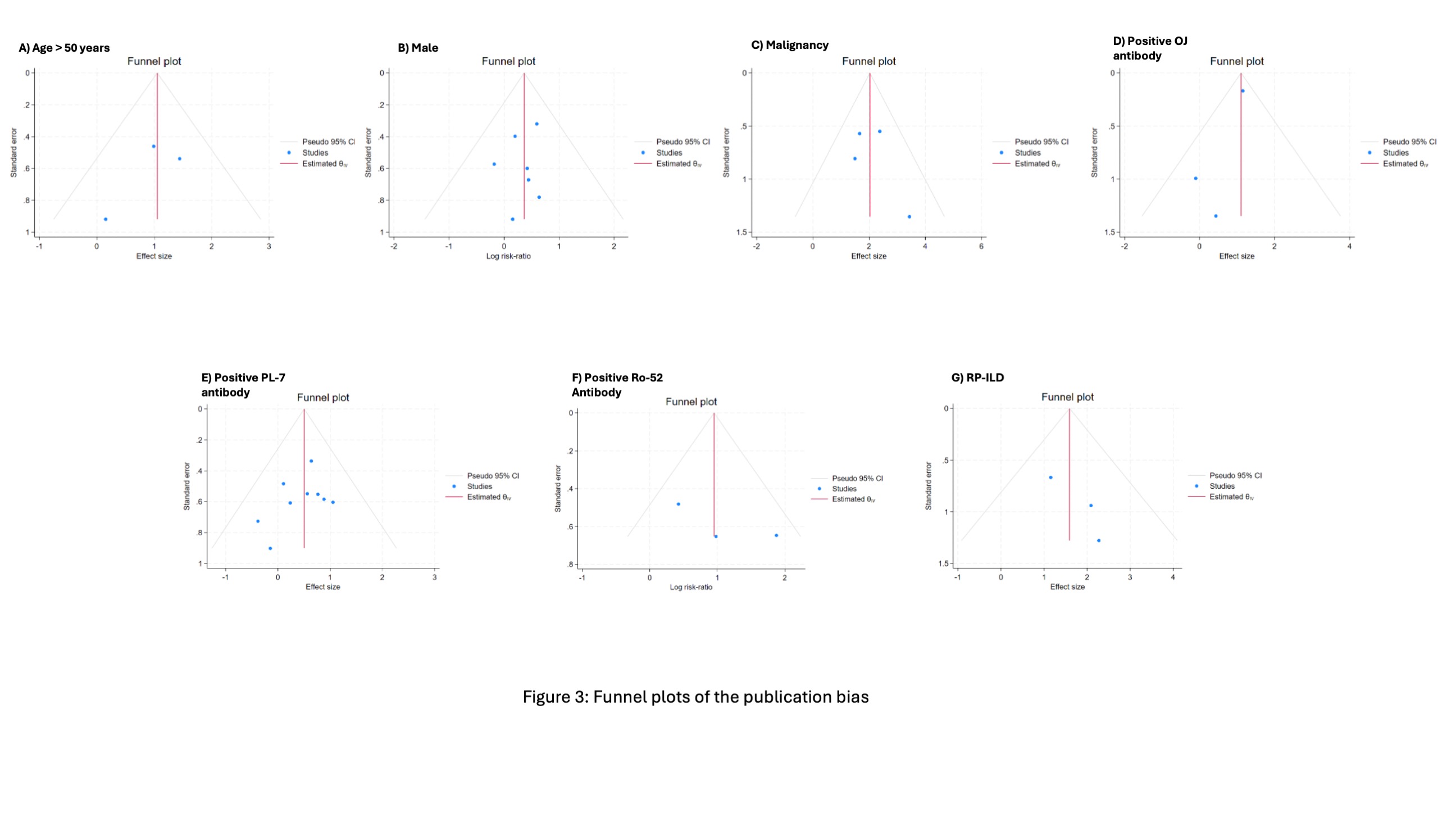 Figure 1: Forest plots of the meta-analysis of the factors affecting mortality risk
Figure 1: Forest plots of the meta-analysis of the factors affecting mortality risk
.jpg) Figure 2: Forest plots of the meta-analysis of the serologies affecting RP-ILD risk
Figure 2: Forest plots of the meta-analysis of the serologies affecting RP-ILD risk
.jpg) Figure 3: Funnel plots of the publication bias
Figure 3: Funnel plots of the publication bias
To cite this abstract in AMA style:
Sodsri T, Chaisrimaneepan N, Thiravetyan B, Boonyawairote R, Mohpichai N, Xanthavanij N, Jakramonpreeya N, Ngamjanyaporn P, Petnak T. Myositis-Specific Antibody Profiles and Factors Associated With Rapidly Progressive Interstitial Lung Disease and Mortality in Antisynthetase Syndrome: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/myositis-specific-antibody-profiles-and-factors-associated-with-rapidly-progressive-interstitial-lung-disease-and-mortality-in-antisynthetase-syndrome-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/myositis-specific-antibody-profiles-and-factors-associated-with-rapidly-progressive-interstitial-lung-disease-and-mortality-in-antisynthetase-syndrome-a-systematic-review-and-meta-analysis/
