Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis presents with multiple joint pains and it is traditionally, examined by the clinicians. The utility of patient self‐joint counts has become an increasingly important area to explore, with remote disease monitoring and telehealth taking on a larger role across rheumatology practices post the global pandemic and increasing scarcity of Rheumatologist in comparison to the increasing case load. This study was inspired from the video released by Centre for Epidemiology and Arthritis on self-assessment of joints in patients with RA to replace clinical examination.
Methods: Sixty-two consecutive patients of RA over the age of 18 who attended our out-patient department between October 2022 and December 2022 were included in this study. We prepared an instructional manual with pictorial representation in English and local language to explain the joint examination to patients. If the patient had difficulty in reading, the attendant was allowed to explain to the patient. A pilot testing was done on ten patients for clarity of understanding, and it was well accepted. Same manual was applied to study participants to maintain uniformity. They marked the tender and swollen joints and the clinical was blinded to their findings. They also scored the pain, difficulty of the questionnaire and patient global assessment score. The patient was then evaluated by an experienced Rheumatologist well versed in RA joint examination.
Results: The total number of joints assessed by patients and clinicians was 3968. The number of joints with either tender or swollen as examined by clinician and patient was 559 and 499, respectively. The sensitivity of patient-reported joint counts was 86.02% (82.6–88.9%), while the specificity was 95.62% (94.8–96.3%). For swollen joints, the sensitivity was 89.2% and the specificity was 96.2%. For tender joints, the sensitivity was 85.04%, and the specificity was 93.8% (Figure 1)Among joint categories, patient self-assessment was more accurate for proximal joints such as the shoulder (specificity 91.95%) and elbows (sp 96.18%). In contrast, distal joints like the wrist, metacarpophalangeal joints, knee, and ankle were assessed more accurately by clinicians. The CDAI was calculated as per clinician and patient tender, swollen joints were calculated individually. There was a strong correlation between CDAI (phy) and CDAI (pt) (rho-0.99).Cronbach’s alpha for CDAI (patient) was 0.701. There was a strong correlation between the total joint counts reported by physicians and patients with higher propensity for swollen joints than tender joints (rho= 0.887 and 0.827, respectively (p < 0.001)) Intraclass correlation coefficients (ICC) for total joints, swollen joints, and tender joints were 0.810, 0.880, and 0.770, respectively, indicating good to excellent reliability.( Figure 2A,2B,2C)
Conclusion: This study shows that with proper training, patient self-assessment of joints is a reliable alternative for online consultations, especially in remote areas. It is particularly accurate for detecting swollen joints, making it useful for remote monitoring and treatment decisions. The findings support integrating self-assessment into telemedicine to improve access and care quality.
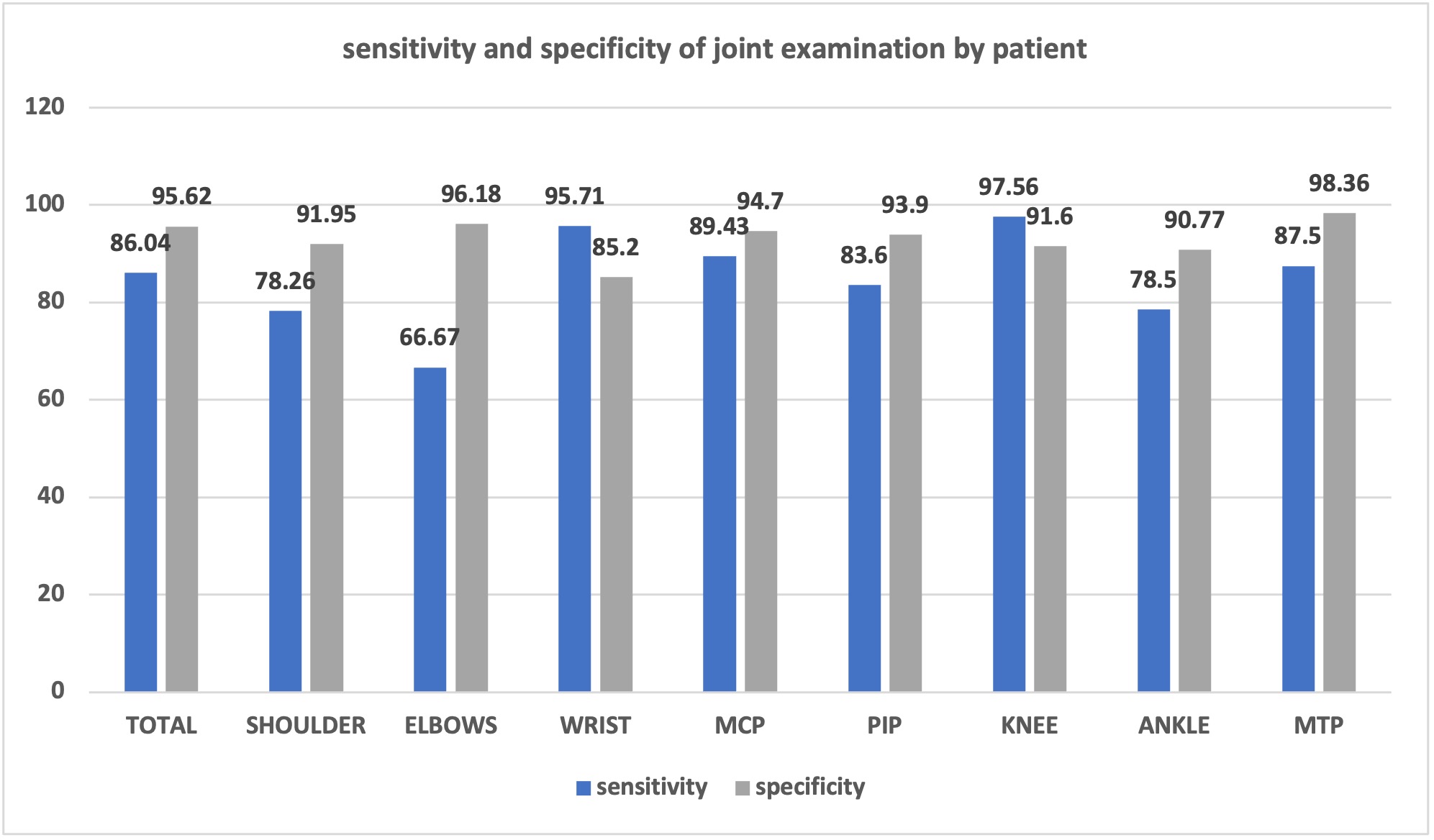 Figure 1: sensitivity and specificity of joint examination by patient
Figure 1: sensitivity and specificity of joint examination by patient
.jpg) Fig 2A: correlation between total number of joints examined by patient vs clinician ; 2B: Correlation between swollen joints examined by patient vs clinician; 2C: Correlation between tender joints examined by patient vs clinician
Fig 2A: correlation between total number of joints examined by patient vs clinician ; 2B: Correlation between swollen joints examined by patient vs clinician; 2C: Correlation between tender joints examined by patient vs clinician
To cite this abstract in AMA style:
Sathiyaseelan S, Kansurkar S, Krishna K, Bhatt V. Bridging the Gap: The Use of Patient Joint Self-Assessment in RA Treatment Response Evaluation [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/bridging-the-gap-the-use-of-patient-joint-self-assessment-in-ra-treatment-response-evaluation/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bridging-the-gap-the-use-of-patient-joint-self-assessment-in-ra-treatment-response-evaluation/
