Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: This study assesses the impact of a clinical pharmacist-directed intervention on medication adherence and clinical outcomes in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis receiving non-infusion disease-modifying antirheumatic drugs (DMARDs). Previous studies on patient education interventions in rheumatology have yielded mixed results due to variability in study populations and educational methods. Pharmacist-led interventions in other chronic diseases, such as hypertension and diabetes, have demonstrated improved disease management and adherence, but data on their effectiveness in inflammatory arthritis remains limited.
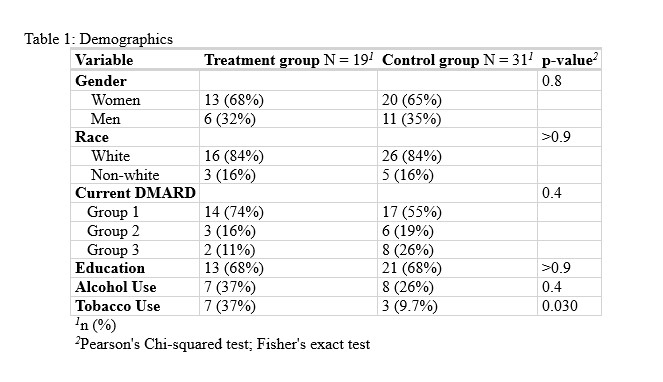
Methods: A prospective, controlled study was conducted from July to December 2024 at Ohio State University (OSU) Rheumatology. Fifty adult patients were enrolled and assigned to either a pharmacist-directed intervention group or a usual care control group. The intervention group received pharmacist-led education, drug toxicity monitoring, and follow-up. Surveys administered at baseline and follow-up included the Morisky Medication Adherence Scale (MMAS), the Routine Assessment of Patient Index Data 3 (RAPID3), and three medication knowledge questions. Statistical analyses included Pearson’s chi-square test for categorical variables and Wilcoxon rank sum test for continuous variables. The primary outcome was MMAS score, with RAPID3 and medication knowledge responses as secondary outcomes.
Results: Baseline characteristics were similar between groups, except for a higher prevalence of tobacco use in the intervention group (p = 0.03). No significant differences were found in MMAS scores (p = 0.84), RAPID3 dichotomous outcomes (p = 0.04), or medication knowledge responses. Participants with higher education levels were more likely to report confidence in their medication knowledge. While the intervention group showed a trend toward improved disease control based on RAPID3 scores, this difference did not reach statistical significance. Correlation analysis revealed associations between gender and DMARD failure (r = 0.37, p < 0.01), race and anti-CCP positivity (r = 0.31, p < 0.05), and tobacco use with education level (r = -0.41, p < 0.01). The strongest correlation was between RF and CCP positivity (r = 0.83, p < 0.001).
Conclusion: Pharmacist-led patient education did not significantly improve medication adherence or clinical outcomes in this small cohort. However, trends in RAPID3 scores suggest a potential benefit in disease control. Confidence in medication knowledge was higher in those with greater educational attainment. Further large-scale studies are warranted to determine the impact of pharmacist-led education in inflammatory arthritis, similar to its demonstrated benefits in other chronic conditions such as hypertension and diabetes.
To cite this abstract in AMA style:
Hurley C, Kotha M, Paul J, Barbee J. Impact of Clinical Pharmacist-Directed Patient Education on Medication Adherence and Clinical Outcomes in Patients with Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-clinical-pharmacist-directed-patient-education-on-medication-adherence-and-clinical-outcomes-in-patients-with-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-clinical-pharmacist-directed-patient-education-on-medication-adherence-and-clinical-outcomes-in-patients-with-inflammatory-arthritis/

.jpg)