Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Key features in the pathophysiology of SLE include cytokine dysregulation and autoantibody production. Traditional autoantibody testing in SLE is primarily limited to intracellular antigens best represented by the ANA and ENA. A novel technique, Rapid Extracellular Antigen Profiling (REAP), enables detection of autoantibodies to extracellular antigens in their 3D conformation via expression in a yeast library. This study investigates the presence of autoantibodies (AAbs) to over 1500 extracellular antigens, including 11 Type A IFNs in longitudinal serum samples from SLE patients and controls.
Methods: Serum Abs were quantified through the REAP assay on over 4000 individual samples from 635 SLE patients, 485 healthy controls and 186 unaffected family members. REAP score reproducibility was assessed by running samples in duplicate, with a resulting high REAP score correlation (median correlation 0.87). Results are a readout of increased antibody binding to an antigen on a scale of 0-4, with higher scores indicating increased binding. Reactivity of the REAP assay was confirmed by ELISA for specific antigens.
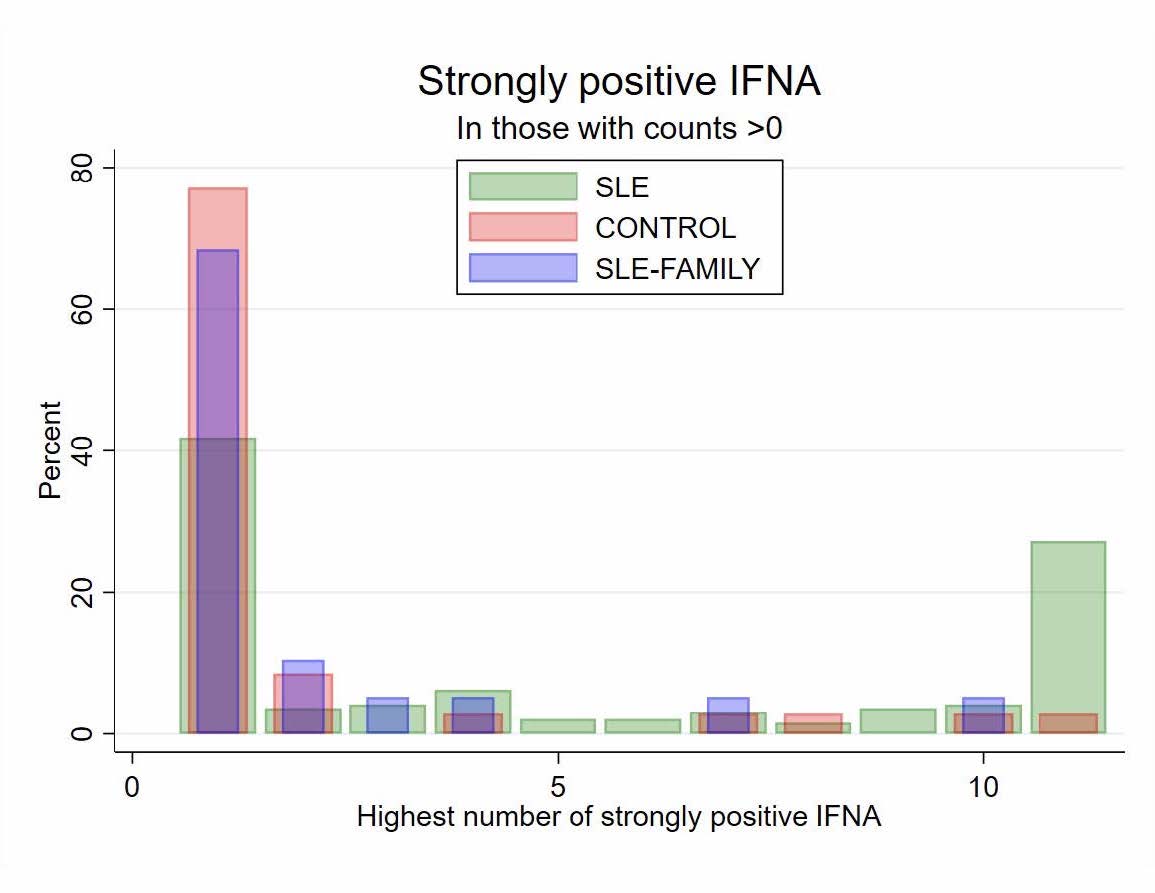
Results: Lupus patient sera had increased numbers of AAbs to extracellular antigens compared to controls. Black SLE patients had increased extracellular AAbs compared to White patients. AAbs were persistent and the number trended to increase over time in sera from SLE patients. There was correlation of AAbs in SLE patients vs first degree relatives. As shown in the volcano plot in Figure 1, there was a markedly higher prevalence of Type I IFN AAbs in SLE sera vs controls and healthy family member sera (36% vs 13%; p= 4.2×10-6). The IFN library included 11 distinct Type I IFNs. Among those with SLE who had Type I interferon reactivity, 28% exhibited reactivity to all 11 Type I IFN (Figure 2 and 3). Only 2 controls exhibited reactivity to all 11 Thpe I IFNs Inhibition assays demonstrated no cross-reactivity between the different IFN antigens, indicating that each AAb reactivity is specific to one of the 11 Type I IFN antigens. Surprisingly, presence of Type I IFN AAbs was not found to be associated with the presence of lupus nephritis nor with increased lupus disease activity as measured by SLEDAI. During 2019-2021 there was an increase in Type I IFN AAbs in control sera but not in the lupus cohort, possibly reflecting COVID vaccination or COVID infection. We are currently testing the sera and controls with or without Type I IFN AAbs for inhibitory activity against Type I IFNs and whether there is a correlation between Type I IFN inhibition with disease activity.
Conclusion: Our study demonstrates a significantly higher prevalence of autoantibodies to extracellular antigens in lupus sera compared to controls. There was a highly significant correlation of type I IFN AAbs in serum of patients with SLE compared to healthy controls. The presence of Type I IFN AAbs overall was not associated with LN or overall disease activity. Further characterization of neutralizing AAbs may yield additional insight into their disease pathogenesis. Further analysis of correlations of lupus manifestations, chronic damage and disease activity is in progress.
 This analysis identifies AAbs associated with SLE compared to healthy controls and unaffected family members, adjusting for age, sex, race. 635 patients with SLE; 485 controls and unaffected family members. Firth (penalized) logistic regression, adjusted for age, sex, race, using baseline sample for each subject. Note significantly higher prevalence of type-I interferon AAbs in patients with SLE. Control antibodies on the left and Lupus antibodies on the right.
This analysis identifies AAbs associated with SLE compared to healthy controls and unaffected family members, adjusting for age, sex, race. 635 patients with SLE; 485 controls and unaffected family members. Firth (penalized) logistic regression, adjusted for age, sex, race, using baseline sample for each subject. Note significantly higher prevalence of type-I interferon AAbs in patients with SLE. Control antibodies on the left and Lupus antibodies on the right.
.jpg) Heat map of antibodies to extracellular antigens in with associated reactivity to intracelluar antigens targeted in lupus. Other reactivities are shown to the left along with the clinical manifestations of the patient at the time the sera was obtained. Notable are the anti-Type I IFN antibodies along with the clustering of reactivity to other extracellular antigens. Clusters of reactivity to one group of antigens is in some cases exclusive to other reactivities
Heat map of antibodies to extracellular antigens in with associated reactivity to intracelluar antigens targeted in lupus. Other reactivities are shown to the left along with the clinical manifestations of the patient at the time the sera was obtained. Notable are the anti-Type I IFN antibodies along with the clustering of reactivity to other extracellular antigens. Clusters of reactivity to one group of antigens is in some cases exclusive to other reactivities
.jpg) Reactivity of each group to the 11 different Type I interferons noting the significantly higher prevalence of autoantibodies in the lupus cohort compared to controls or family members especially at the higher levels of number of antibodies to the Type I interferons in lupus
Reactivity of each group to the 11 different Type I interferons noting the significantly higher prevalence of autoantibodies in the lupus cohort compared to controls or family members especially at the higher levels of number of antibodies to the Type I interferons in lupus
To cite this abstract in AMA style:
Counts K, Wilson D, Furchtgott L, Gilkeson G. Autoantibodies to Extracellular Antigens in Lupus Patients Serum Versus Controls; Predominance of Autoantibodies to Type I Interferons in Lupus Sera [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/autoantibodies-to-extracellular-antigens-in-lupus-patients-serum-versus-controls-predominance-of-autoantibodies-to-type-i-interferons-in-lupus-sera/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibodies-to-extracellular-antigens-in-lupus-patients-serum-versus-controls-predominance-of-autoantibodies-to-type-i-interferons-in-lupus-sera/
