Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease with widespread clinical manifestations. Neuropsychiatric SLE (NPSLE), a complex and poorly understood subset of SLE, comprises of 19 conditions with high rates of morbidity and mortality. Included in the spectrum of NPSLE is transverse myelitis (TM), a neuro-inflammatory disorder characterized by rapid-onset motor and sensory deficits. In this study, we aim to investigate the prevalence of TM among the general SLE population and to compare clinical characteristics and outcomes between SLE patients with and without TM.
Methods: A retrospective chart review was conducted utilizing data from the TriNetX global research network platform, a health record electronic database. A total of 135,027 patients with SLE (ICD-10: M32) were identified across 97 health care organizations, of which 1,224 patients had a diagnosis of transverse myelitis (ICD-10: G37.3 or G04.9) and 133,803 patients did not have transverse myelitis. A 1:1 propensity score matching was done using 60 demographic and clinical variables, and yielded two cohorts of 1,219 patients each. The variables studied included baseline patient demographics, clinical manifestations/comorbidities, and autoantibody profile. Outcomes analyzed included mortality, laboratory findings, and medication usage. Kaplan-Meier curve and log-rank test were used for survival analysis. Statistical significance was defined as a p-value of < 0.05.
Results: The prevalence of TM among the general SLE population was 0.91%. Analysis of the demographic data before propensity matching revealed higher rates of TM in male (p=0.019), African-American, and Asian patients ( p-values < 0.001). Clinical manifestations such as glomerular disease, thrombosis, other neurological involvement including seizures, psychosis and neuromyelitis optica (NMO), as well as various hematological lab abnormalities were more frequent in the TM group prior to matching (all p-values < 0.001). The frequencies of Ro/SSA, La/SSB, Ribosomal-P (all p-values < 0.001), RNP (p=0.009), DsDNA antibodies (p=0.020), as well as low C3 and C4 complements (p< 0.001) were significantly higher in TM patients before matching (Table 1 and 2).After propensity matching, neurological manifestations such as myasthenia (p=0.002) and NMO (p< 0.001) as well as the frequency of La/SSB antibody (p=0.030) were significantly higher in the TM SLE group (Table 1 and 2).Kaplan-Meier survival analysis revealed that TM is a significantly poor prognostic factor in SLE patients, with lower survival probability compared to patients without TM (HR: 1.423, 95% CI:1.11-1.82). During the study period, 14.2% of patients with TM died and 8.1% of patients without TM died (RR: 1.75, 95% CI: 1.38-2.21) (Figure 1A and 1B).
Conclusion: Transverse myelitis is a rare, but significant complication of SLE and with a poor prognostic factor in SLE patients. TM was also associated with distinct antibody profiles and clinical manifestations/comorbid conditions, especially other NPSLE findings. Given the risk of profound neurological deficits, early diagnosis and treatment is of the utmost importance to help improve long-term outcomes.
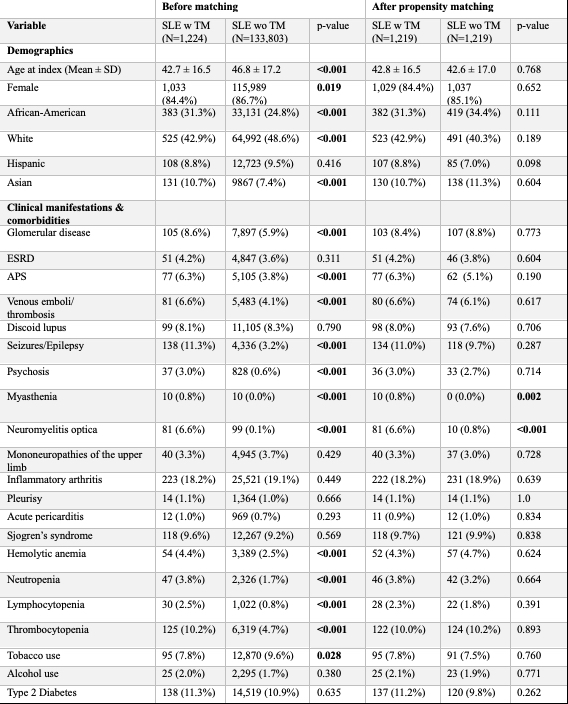 Table 1: Demographic Characteristics and Clinical Manifestations/Comorbidities of Patients With Systemic Lupus Erythematosus With and Without Transverse Myelitis Before and After Propensity Matching.
Table 1: Demographic Characteristics and Clinical Manifestations/Comorbidities of Patients With Systemic Lupus Erythematosus With and Without Transverse Myelitis Before and After Propensity Matching.
.jpg) Table 2: Medication Treatment and Autoantibody Profile of Patients With Systemic Lupus Erythematosus With and Without Transverse Myelitis Before and After Propensity Matching.
Table 2: Medication Treatment and Autoantibody Profile of Patients With Systemic Lupus Erythematosus With and Without Transverse Myelitis Before and After Propensity Matching.
.jpg) Figure 1A: Survival Probability in Systemic Lupus Erythematosus With and Without Transverse Myelitis Using Kaplan-Meier Survival Analysis.
Figure 1A: Survival Probability in Systemic Lupus Erythematosus With and Without Transverse Myelitis Using Kaplan-Meier Survival Analysis.
Figure 1B: Mortality Rate Data in Systemic Lupus Erythematosus With and Without Transverse Myelitis.
To cite this abstract in AMA style:
Daneshvar A, Tiwana A, Nachawati D, Pfeil K, Harper E, Frumker L, Gump M, Pamuk O. Transverse Myelitis in Systemic Lupus Erythematosus: Disease Manifestations and Clinical Outcomes from Multi-Center Data [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/transverse-myelitis-in-systemic-lupus-erythematosus-disease-manifestations-and-clinical-outcomes-from-multi-center-data/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/transverse-myelitis-in-systemic-lupus-erythematosus-disease-manifestations-and-clinical-outcomes-from-multi-center-data/
