Session Information
Date: Sunday, October 26, 2025
Session Type: Abstract Session
Session Time: 4:00PM-4:15PM
Background/Purpose: Lupus Nephritis (LN) is one of the most serious complications of SLE (Systemic Lupus Erythematosus) characterized by an attack of the kidneys by the immune system which typically develops within 5 years of the initial diagnosis of SLE. It is suspected that up to 60% of those with SLE develop kidney-related complictions. Some complications of Lupus Nephritis include kidney failure requiring dialysis or transplantation, among other cardiovascular complications. Many medications exist for the management of some of the comorbidities associated with LN patients, but not much is known on the benefits on the condition itself. An observational, retrospective cohort study was designed which aimed to evaluate the effect of GLP-1 (glucagon-like peptide-1) agonists compared to SGLT2 (sodium-glucose cotransporter-2) inhibitors on the outcomes in patients with Lupus Nephritis using the TriNetX database which included electronic healthcare records from over 142 global collaborative healthcare organizations.
Methods: The study utilized patients 18 years or older with a diagnosis of LN (Lupus Nephritis) using the International Classification of Diseases, Tenth Revision (ICD-10) codes. Two different cohorts were created: the first cohort consisted of patient with LN who were on SGLT2 inhibitors, and the second cohort consisted of patients with LN who were on GLP-1 agonists. The index event in study was defined as the initial diagnosis of LN, later followed by three years of exposure to either SGLT-2 inhibitors or GLP-1 agonists. Propensity matching was used for the age at index, gender, race/ethnicity, comorbidities (hypertension, obesity, diabetes, tobacco use), and medications (DMARDS, steroids, biologics, statins, aspirin).
Results: A total of 1,375 patients with LN on SGLT2 inhibitors, and 1,034 patients with LN on GLP-1 agonists were reviewed. Before propensity matching was performed, patients on SGLT2 inhibitors were older (mean age of 51.9 vs. 48.2), consisted of more females (1,043 vs. 884), had more patients with hypertension (1,170 vs. 837), and consisted of mostly Black/African American patients when compared to the GLP-1 agonist group which consisted of mostly White patients. After propensity matching, 1,021patients were excluded, and a total of 694 patients remained in each group. Results showed that the group of patients with LN who were on GLP-1 agonists had reduced progression of chronic kidney disease (RR: 1.526, 95% CI: 1.179-1.976, p= 0.0014), decreased mortality (RR: 2, 95% CI: 1.239-3.227, p=0.0037), and a decreased risk of acute myocardial infarctions (RR: 2.248, 95% CI: 1.294-3.904, p=0.0030).
Conclusion: The findings suggest that patients with Lupus Nephritis taking GLP-1 receptor agonists have a reduced risk of mortality, acute myocardial infarctions, and a decreased progression of CKD compared to patients taking SGLT-2 inhibitors. Further research should be conducted with larger groups, and with longer follow up time to confirm and possibly explain any potential explanations or contributing factors.
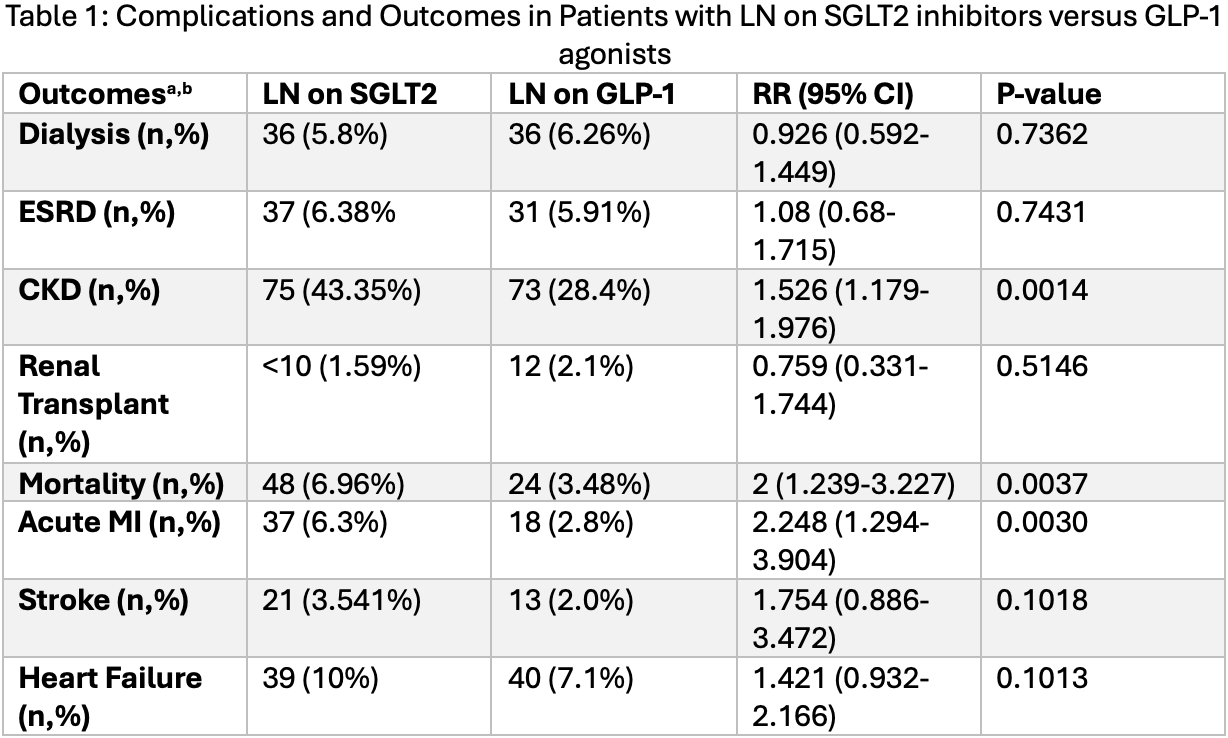 Abbreviations: Acute MI: Acute Myocardial Infarction, CKD: Chronic Kidney Disease, ESRD: End-Stage Renal Disease, GLP-1: glucagon-like peptide-1 agonists, LN: Lupus Nephritis, RR: Relative Risk, SGLT 2: sodium-glucose cotransporter-2 inhibitors, 95% CI: 95% Confidence Interval ; a- Propensity matched cohorts based on baseline demographics, comorbidities, and medication use. ; b- All patients with outcomes that occurred prior to the time window were excluded from our cohorts.
Abbreviations: Acute MI: Acute Myocardial Infarction, CKD: Chronic Kidney Disease, ESRD: End-Stage Renal Disease, GLP-1: glucagon-like peptide-1 agonists, LN: Lupus Nephritis, RR: Relative Risk, SGLT 2: sodium-glucose cotransporter-2 inhibitors, 95% CI: 95% Confidence Interval ; a- Propensity matched cohorts based on baseline demographics, comorbidities, and medication use. ; b- All patients with outcomes that occurred prior to the time window were excluded from our cohorts.
To cite this abstract in AMA style:
Grzybowski K, Tan I. Comparing the Impact of GLP-1 Agonists and SGLT-2 Inhibitors on Outcomes in Lupus Nephritis: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/comparing-the-impact-of-glp-1-agonists-and-sglt-2-inhibitors-on-outcomes-in-lupus-nephritis-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-the-impact-of-glp-1-agonists-and-sglt-2-inhibitors-on-outcomes-in-lupus-nephritis-a-retrospective-cohort-study/
