Session Information
Date: Sunday, October 26, 2025
Session Type: Abstract Session
Session Time: 3:15PM-3:30PM
Background/Purpose: Complete renal response (CRR) and flare prevention, as early markers of long-term kidney survival, are important outcomes in lupus nephritis (LN) clinical trials.
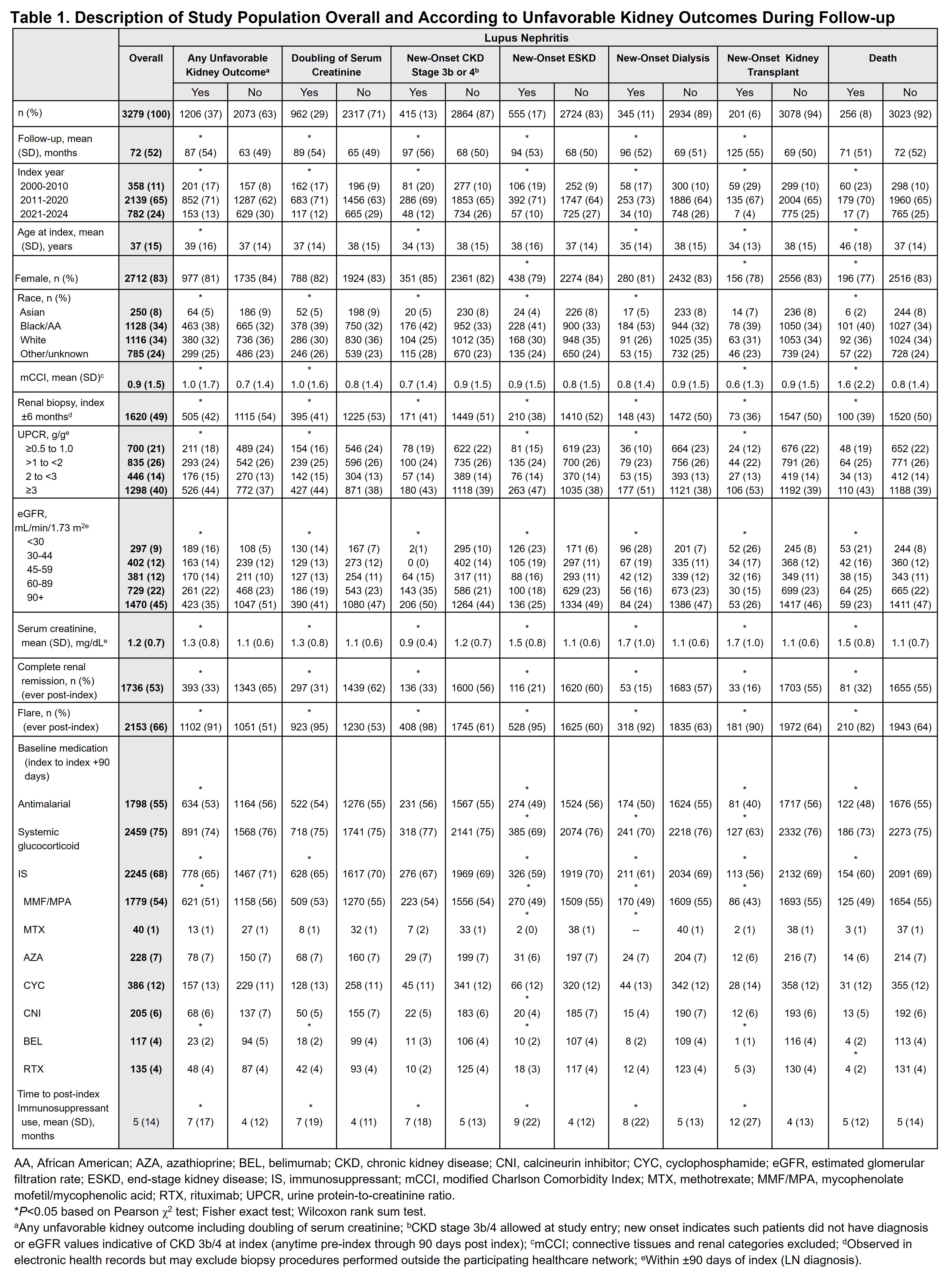
Methods: This US-based retrospective cohort study (January 1, 2000 to October 15, 2024) used deidentified patient-level electronic health records from a national network of healthcare organizations (118 million patients) to assess time to initial CRR, LN flare, estimated glomerular filtration rate (eGFR) slope and unfavorable kidney outcomes. Patients were ≥18 years old with newly diagnosed LN (index), had baseline urine protein-to-creatinine ratio (UPCR) and eGFR within 90 days of index plus an additional UPCR and eGFR >90 days post index. Patients were required to have a baseline UPCR of ≥0.5 g/g. Patients with pre-existing end-stage kidney disease (ESKD), dialysis or kidney transplant were excluded. CRR was defined as UPCR < 0.5 g/g and eGFR ≥85% of baseline and no pre-CRR ESKD, dialysis or kidney transplant. LN flare was defined as eGFR decrease of >20%, increase in UPCR of >1 g/g if UPCR < 0.2 g/g or >2.0 g/g if UPCR ≥0.2 g/g or doubling if UPCR >1 g/g compared with baseline or receipt of intravenous methylprednisolone ≥100 mg within 14 days of a LN/systemic lupus erythematosus (SLE) diagnostic code. Unfavorable kidney outcomes included doubling of serum creatinine, new-onset chronic kidney disease (CKD) stage 3b/4, ESKD, dialysis, transplant and death. Week 52, 76 and 104 sub-cohorts included patients with follow-up data and ≥1 UPCR and eGFR during the post-index Week 52, 76 and 104 (±90 days) periods.
Results: Of 3279 patients, unfavorable kidney outcomes occurred in 37% and were more frequent in the following patients: older, longer disease duration, Black, greater comorbidities and poor baseline renal function Mean time in months (mo) from pre-index SLE diagnosis to index was 23 (SD 40). Baseline kidney biopsy (index ±6 mo) occurred in 49% of patients and more frequently in those diagnosed after 2021, with higher baseline UPCR, subsequent CRR and less frequent unfavorable kidney outcomes (P< 0.001). Immunosuppressant (IS) use (index +90 days) was 68%; mean time post-index to IS use, mo (SD) was: 5 (14); and a longer time to IS treatment was associated with poor outcomes (Table 1). Mean time from index to event, mo (SD) was: doubling of serum creatinine, 35 (33); CKD stage 3b/4, 38 (37); ESKD, 42 (37); dialysis, 46 (38); transplant, 65 (44) and death, 61 (46).CRR was achieved in 53% of patients; mean time to initial CRR, mo (SD) was 16 (19) and varied by baseline UPCR (Figure 1a). CRR at Week 52, 76 and 104 was 36%, 38% and 38% respectively. Figure 1b shows median time to initial flare. Figure 1c shows time to event according to 20, 30 and 40% eGFR decline. Figure 1d shows time to unfavorable kidney outcome.Patients who achieved CRR were significantly less likely to experience an unfavorable kidney outcome or flare (Table 2).
Conclusion: Achieving CRR significantly reduced future severe kidney outcomes; however, a minority of patients who achieved CRR at Week 52, 76 or 104 had disease progression. Patients with high baseline UPCR had delayed CRR and those with longer time to initial IS treatment had worse long-term outcomes.
To cite this abstract in AMA style:
Lindsay L, Wang S, Trinh H, Huang Y, Pendergraft W, Rovin B. Complete Renal Response and Long-Term, Progression-Free Survival in Adult Patients With Lupus Nephritis: A Retrospective Cohort Study in the United States [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/complete-renal-response-and-long-term-progression-free-survival-in-adult-patients-with-lupus-nephritis-a-retrospective-cohort-study-in-the-united-states/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/complete-renal-response-and-long-term-progression-free-survival-in-adult-patients-with-lupus-nephritis-a-retrospective-cohort-study-in-the-united-states/

.jpg)
.jpg)