Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Childhood obesity is a global public health concern that impacts the health and wellbeing of all children and particularly negatively affects children living with chronic autoimmune disease. Studies in adults have shown a significant association between obesity and ankylosing spondylitis (AS); however, the association of obesity with juvenile spondyloarthritis (JSpA) is unknown. Obesity may be a risk factor for or a consequence of JSpA. This study aims to evaluate the prevalence of obesity in children with JSpA compared to a healthy control population.
Methods: This retrospective cohort study included 190 children with JSpA and 760 healthy controls. Data on JSpA cases were drawn from a preexisting disease registry and included patients at their initial visit who met one of the following criteria: magnetic resonance imaging (MRI)-defined sacroiliitis, enthesitis-related arthritis (ERA), psoriatic arthritis (PsA), or undifferentiated arthritis. The healthy control group consisted of children without juvenile arthritis derived from the CDC National Center for Health Statistics’ National Health and Nutrition Examination Survey. Cases and controls were matched by sex, race, and age, at a 4:1 ratio. Body mass index (BMI) categories were defined using CDC percentiles: obese (≥95th), overweight (85th–94th), healthy weight (5th–84th), and underweight (< 5th). BMI-for-age z-scores were calculated using the CDC 2000 growth reference in Stata and adjusted for age and sex. A Wilcoxon rank-sum test was used to compare BMI z-scores and chi-square tests assessed differences in BMI categories between children with JSpA and controls.
Results: A total of 950 children were included in the study, of whom 190 had JSpA and 760 were healthy controls. Cohort demographics are presented in Table 1. The distribution of BMI categories was significantly different between JSpA and the matched controls (P < 0.001). As shown in Table 2, a higher proportion of children with JSpA were underweight (26.8% in JSpA vs. 4.2% in controls), while fewer were classified as obese (11.6% in JSpA vs. 22.2% in controls). Histograms comparing BMI-for-age z-scores between children with JSpA and healthy controls are shown in Figure 1. The median BMI z-score was 0.37 (IQR -0.22 to 1.13) for JSpA cases and 0.76 (IQR -0.06 to 1.63) for healthy controls (P = 0.01).
Conclusion: Children with JSpA had significantly lower BMI z-scores compared to age, sex, and race-matched controls. More children with JSpA were underweight when compared with a control population. The impact of disease duration, disease activity, and concurrent medications on BMI in JSpA should be further explored.
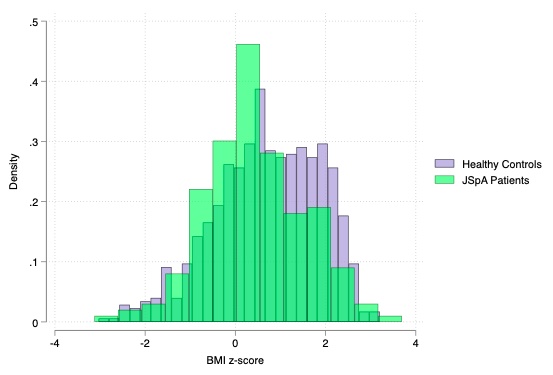 Table 1. Characteristics of children with JSpA versus healthy controls. ^ Subjects with sacroiliitis had MRI-defined inflammation but did not fulfill ILAR criteria for ERA or PsA. * Subjects with undifferentiated arthritis met ERA criteria but had a first-degree relative with psoriasis or met PsA criteria but had a diagnosis of sacroiliitis and inflammatory bowel disease.
Table 1. Characteristics of children with JSpA versus healthy controls. ^ Subjects with sacroiliitis had MRI-defined inflammation but did not fulfill ILAR criteria for ERA or PsA. * Subjects with undifferentiated arthritis met ERA criteria but had a first-degree relative with psoriasis or met PsA criteria but had a diagnosis of sacroiliitis and inflammatory bowel disease.
.jpg) Table 2. Comparison of BMI Categories in children with JSpA versus healthy controls.
Table 2. Comparison of BMI Categories in children with JSpA versus healthy controls.
.jpg) Figure 1. Histograms comparing BMI-for-age z-scores between children with juvenile spondyloarthritis (JSpA) and healthy controls. The median BMI z-score was 0.37 (IQR -0.22 to 1.13) for JSpA cases and 0.76 (IQR -0.06 to 1.63) for healthy controls (P = 0.01).
Figure 1. Histograms comparing BMI-for-age z-scores between children with juvenile spondyloarthritis (JSpA) and healthy controls. The median BMI z-score was 0.37 (IQR -0.22 to 1.13) for JSpA cases and 0.76 (IQR -0.06 to 1.63) for healthy controls (P = 0.01).
To cite this abstract in AMA style:
Baggett K, Brandon T, Weiss P. The Association of Obesity with Juvenile Spondyloarthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-association-of-obesity-with-juvenile-spondyloarthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-of-obesity-with-juvenile-spondyloarthritis/
