Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Toll-like receptors (TLRs) are pattern-recognition receptors of the innate immune response and are important in driving the initial activation of myeloid lineage cells to both pathogenic and non-pathogenic challenges. Deficiency of TLR3, TLR4, or CD14 (a TLR co-receptor) have been shown to mitigate OA progression and pain in animal models. However, the role of TLR signaling in human knee OA (KOA) is less studied. We evaluated the levels of synovial fluid (SF) markers including sTLR4 and sCD14 from patients enrolled in a clinical trial testing the impact of corticosteroid injections to determine if these markers could predict those that are most likely to respond to injections.
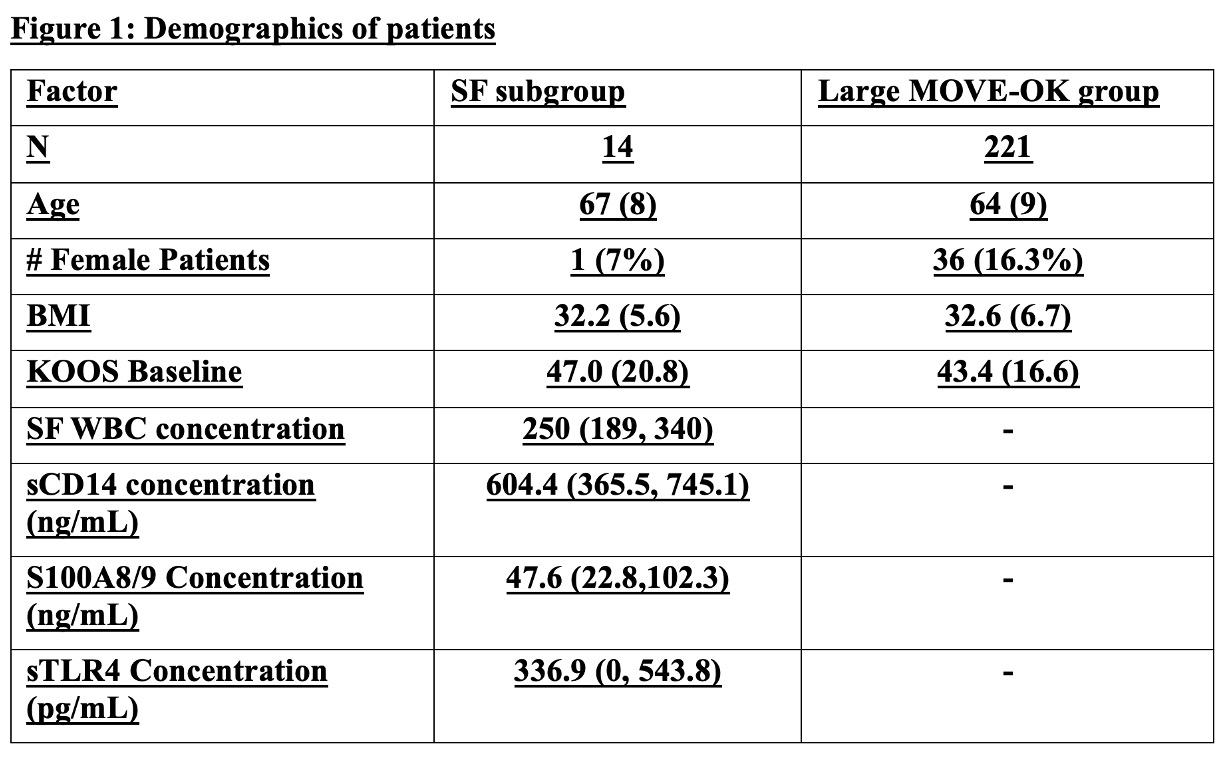
Methods: The MOVE-OK trial was a VA-funded, a multi-center blinded crossover randomized trial, comparing the effects of corticosteroid + lidocaine vs. lidocaine-only injections in Veterans with KOA . Inclusion criteria included a clinical diagnosis of KOA with a K-L X-ray grade ³1, aged 40-80 years, and a clinical indication for joint injection according to the treating provider. 221 participants were randomized to receive blinded corticosteroid (CS) injections plus lidocaine (LC) (40 mg methylprednisolone) or LC-only injections then crossed-over to the other injection at 16 weeks. The primary outcome was the change in the total KOOS measured bi-weekly between 0 and 12 weeks after each injection. 196 participants received both injections, and SF was collected at the time of injection from a total of 40 patients with 14 patients having fluid collected at both injection timepoints. We performed ELISAs on SF from these 14 patients measuring sTLR4, sCD14, and S100A8/9. Associations between SF biomarkers and the change in KOOS was assessed using linear regression incorporating generalized estimating equations to evaluate all time-points (2-12 weeks) after each injection, adjusting for the baseline KOOS score.
Results: Patients included in this subanalysis exhibited similar demographics to those enrolled in the main study (Table 1). SF from 4 patients had sTLR4 concentration below the limit of detection, but otherwise analytes were detectable in all samples. The median (IQR) concentrations of sCD14, S100A8/9 and sTLR4 are shown in Table 1. Patients with high SF WBC counts at baseline were less likely to show improvement in their KOOS scores over the course of the study (Figure 2). A similar trend was shown for sTLR4 concentration in SF. While there was numerically less improvement in KOOS over time between patients with high vs. low concentrations of sCD14 and S100A8/9, differences were not significant. There were no interactions to suggest that the association between biomarkers and the change in KOOS score differed between those receiving a CS v. LC-only injection.
Conclusion: Our results suggest that patients with higher SF levels of WBC and sTLR4 demonstrate less improvement in response to knee injection. Future proteomic analyses of these samples are planned and may provide additional insights. Analysis of these markers in larger cohorts are needed to validate these findings, but our results point to a potential importance of inflammation and the innate immune response in the joint in predicting symptom improvement in response to interventions.
To cite this abstract in AMA style:
Murphy L, Hu B, Nguyen V, England B, Wysham K, Quinones M, Baker J, Scanzello C. High synovial fluid leukocyte counts and markers of TLR activation correlate with poorer response to injections in patients with knee OA [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/high-synovial-fluid-leukocyte-counts-and-markers-of-tlr-activation-correlate-with-poorer-response-to-injections-in-patients-with-knee-oa/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-synovial-fluid-leukocyte-counts-and-markers-of-tlr-activation-correlate-with-poorer-response-to-injections-in-patients-with-knee-oa/

.jpg)