Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Malignancies are one of the leading causes of non-systemic sclerosis-related mortality in patients with systemic sclerosis (SSc)1, with lung cancer being the most common type2,3,4. Although factors such as prolonged immunosuppression4, family history of malignancy5, and smoking6 have been implicated, findings have been inconsistent. We conducted a matched case-control study to investigate clinical, serological, and treatment-related risk factors associated with lung cancer among patients with SSc in a Michigan-based cohort.
Methods: Data were extracted retrospectively using DataDirect, a self-service tool that retrieves information from the electronic medical record system by identifying relevant International Classification of Diseases (ICD) 9 and 10 codes for SSc and lung cancer (710.1, 162.9 and M34.0, M34.1, M34.2, M34.8, M34.9, C34.00-C34.92, respectively) and/or listed diagnosis in the medical record. Inclusion criteria included adults aged 18 or older who were actively followed by rheumatology at the University of Michigan and had a confirmed diagnosis of SSc, either by fulfillment of the ACR classification criteria or through clear documentation in a rheumatologists’ note. Exclusion criteria were patients aged under 18, lack of active follow-up at the University of Michigan, localized scleroderma, or secondary lung cancer (metastatic, with a primary site other than lung). Using these criteria, we identified 102 patients: 51 SSc patients with lung cancer (cases) and 51 age-matched SSc patients without lung cancer (controls). Paired t-tests, McNemar’s and Bowker’s symmetry tests were used to assess baseline differences. Conditional logistic regression was then performed to examine associations with lung cancer.
Results: Baseline patient data characteristics are summarized below in table 1. Compared to controls, cases had significantly higher rates of diffuse cutaneous SSc (72.5% vs. 39.2%, p=0.0036), former smoking (64.7% vs. 27.5%, p=0.0009), presence of lung nodules on CT chest (87.5% vs. 61.2%, p=0.0164), and immunosuppressive therapy use (89.4% vs. 56.9%, p=0.0006). Mean DLCO% was significantly lower in cases (48.7% vs. 61.1%, p=0.0011). In multivariable analysis (table 2), former smoking (OR 8.22, 95% CI: 2.39 – 28.27, p=0.0008), glucocorticoid use (OR 14.50, 95% CI: 3.46 – 60.77, p=0.0003), and nodules on chest CT (OR 3.2, 95% CI: 1.17 – 8.74, p=0.0232) were independently associated with lung cancer. Diffuse cutaneous subtype was a risk factor, while limited cutaneous SSc was protective (OR 0.14, 95% CI: 0.04 – 0.49, p=0.0017). DLCO% was inversely associated with lung cancer risk (OR 0.95 per % increase, 95% CI: 0.92 – 0.99, p=0.0065). Cases had 1300% higher odds of death (OR 14%, 95% CI: 3.34 – 58.77, p=0.0003).
Conclusion: In this matched cohort, lung cancer in SSc was significantly associated with diffuse cutaneous subtype, prior smoking history, nodules on CT chest, reduced DLCO, and glucocorticoid exposure. In contrast, limited cutaneous SSc conferred a protective effect. These findings underscore the importance of clinical phenotype and treatment history in assessing malignancy risk in SSc patients and support the need for targeted cancer screening protocols.
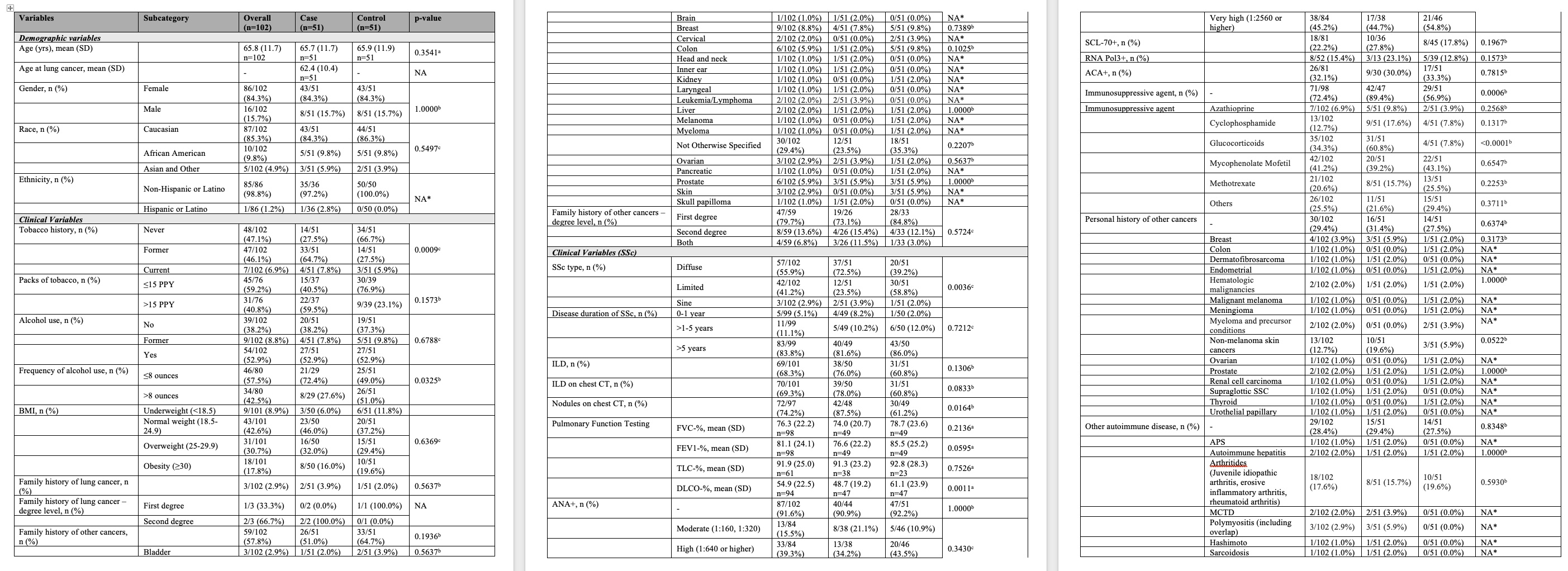 Table 1a: Baseline Characteristics
Table 1a: Baseline Characteristics
.jpg) Table 1b: Baseline Characteristics
Table 1b: Baseline Characteristics
.jpg) Table 2: Conditional Logistic Regression
Table 2: Conditional Logistic Regression
To cite this abstract in AMA style:
Siddiqui M, Chen Y, Gedert R, Huang S, Khanna D, Varga J. Risk Factors and Clinical Predictors of Lung Cancer in Systemic Sclerosis: A Matched Case-Control Study from a Michigan Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/risk-factors-and-clinical-predictors-of-lung-cancer-in-systemic-sclerosis-a-matched-case-control-study-from-a-michigan-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-and-clinical-predictors-of-lung-cancer-in-systemic-sclerosis-a-matched-case-control-study-from-a-michigan-cohort/
