Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatologists and primary care providers (PCPs) are some of the most trusted clinicians for people living with autoimmune rheumatic diseases (AIRD), and they may influence the vaccine decision-making process during outpatient visits. We aimed to determine the factors associated with receipt of a COVID-19 vaccine during the immediate follow-up interval after either rheumatology or PCP clinic visits.
Methods: We used electronic health records (EHR) to conduct a retrospective cohort study of established patients with AIRD at our institution seen from 12/8/2020 through 1/8/2024. We conducted two separate cohort analyses in patients who had 2+ clinic visits in the observation period with (1) rheumatology or (2) a PCP. The primary outcome of “post-visit vaccination” was defined as receipt of a dose of the COVID-19 vaccine during the 8-day interval after a rheumatology or a PCP clinic visit (i.e., the day of visit + 7 days post-visit). We built multivariable logistic regression models to identify factors independently associated with post-visit vaccine receipt. Secondarily, we conducted a self-controlled case series (SCCS) analysis to compare receipt of COVID-19 vaccination during the 8-days post-visit “hazard interval” vs. 8-days pre-visit “control interval”, and censored at the time of their vaccine receipt or death during these intervals.
Results: We identified 2,628 individuals with rheumatology (Table 1) and 493 individuals with PCP clinic visits, of whom 440 (16.7%) and 119 (24.1%) received a COVID-19 vaccine in the 8-day post-visit interval, respectively. In the multivariable logistic regression model examining the outcome following rheumatology visits, older age (OR=1.17, 95% CI 1.03 – 1.33, for every 10-year increase), Black race (OR=1.49, 95% CI 1.15 – 1.92), and use of glucocorticoids (OR=1.63, 95% CI 1.25 – 2.14), immunosuppressives (OR=1.40, 95% CI 1.03 – 1.88), and intravenous immunoglobulin (OR=1.91, 95% CI 1.16 – 3.16) were associated with higher odds of post-visit vaccine receipt (Figure 1a). Among eligible patients with PCP clinic visits, only older age (OR=1.58, 95% CI 1.22 – 2.06) and Black race (OR=1.70, 95% CI 1.06 – 2.72) were associated with a post-visit vaccine receipt (Figure 1b). In the SCCS analysis, there were significantly higher rates of vaccine receipt during the post-visit hazard interval compared to each person’s control interval following rheumatology (IRR=1.87, 95% CI 1.62 – 2.18, p< 0.0001) and PCP clinic visits (IRR=3.81, 95% CI 2.75 – 5.36, p< 0.0001); among only patients who received a vaccine, the rates were similar.
Conclusion: In this cohort study of patients with AIRD, we found that older age, Black race, and use of certain high-risk medications were associated with higher odds of COVID-19 vaccination in close proximity to a visit with a rheumatologist or PCP. While both PCP and rheumatology clinic visits were associated with more post-visit COVID-19 vaccinations, our results suggest that rheumatologists may be focusing vaccination efforts among those with certain high-risk patient characteristics such as older age or greater immunosuppression burden. Effective interventions aimed at improving vaccine uptake could be implemented at or soon after a clinic visit.
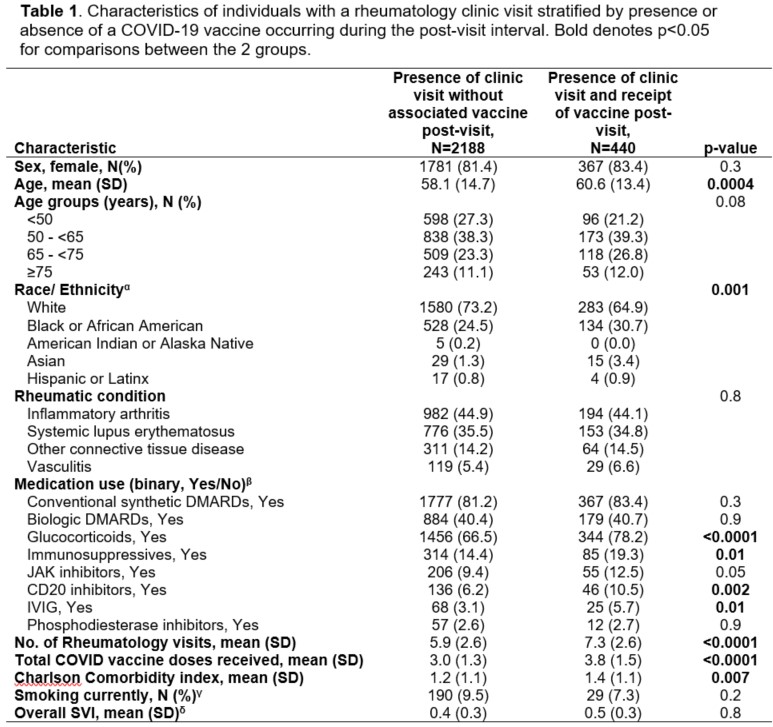 αmissing for 33 individuals. βcategories are not mutually exclusive. γmissing for 222 individuals. δmissing for 266 individuals. Rheumatology visits were defined as an outpatient visit occurring with a rheumatologist during the timeframe from Dec. 8, 2020 through Jan. 8, 2024. AIRD, autoimmune rheumatic diseases; DMARDs, disease-modifying antirheumatic drugs; IVIG, intravenous immunoglobulin; JAK, janus kinase; SD, standard deviation; SVI, social vulnerability index.
αmissing for 33 individuals. βcategories are not mutually exclusive. γmissing for 222 individuals. δmissing for 266 individuals. Rheumatology visits were defined as an outpatient visit occurring with a rheumatologist during the timeframe from Dec. 8, 2020 through Jan. 8, 2024. AIRD, autoimmune rheumatic diseases; DMARDs, disease-modifying antirheumatic drugs; IVIG, intravenous immunoglobulin; JAK, janus kinase; SD, standard deviation; SVI, social vulnerability index.
.jpg) Figure 1. Results of multivariable logistic regression model with odds ratio (OR) and 95% confidence intervals (CI) for covariates associated with receipt of a COVID-19 vaccine during the 8-day post-visit interval after an outpatient a) rheumatology clinic visit or b) primary care clinic visit.
Figure 1. Results of multivariable logistic regression model with odds ratio (OR) and 95% confidence intervals (CI) for covariates associated with receipt of a COVID-19 vaccine during the 8-day post-visit interval after an outpatient a) rheumatology clinic visit or b) primary care clinic visit.
Model includes all relevant covariates of biological significance (e.g., sex, age) and those with p < 0.25 in the univariable analysis. OR and CI presented on a logarithmic scale. aOR, adjusted odds ratio; IVIG, intravenous immunoglobulin; JAK inhibitor, janus kinase inhibitor.
To cite this abstract in AMA style:
Jackson L, Wright N, Begum R, Rahman F, Patel R, Saag K, Curtis J, Danila M. Influence of Outpatient Clinic Visits on Receipt of the COVID-19 Vaccine among People with Autoimmune Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/influence-of-outpatient-clinic-visits-on-receipt-of-the-covid-19-vaccine-among-people-with-autoimmune-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influence-of-outpatient-clinic-visits-on-receipt-of-the-covid-19-vaccine-among-people-with-autoimmune-rheumatic-diseases/
